Advances in Malignant Lymphoma Virtual Meeting: Stratifying Risk, Targeting Precursor Cells, Hacking the Epigenome, and More
Virtual scientific meetings have become the “new normal” in the COVID-19 era, enabling researchers to present and discuss recent advances in their respective fields, facilitating potential collaborations and conversations, and ultimately allowing science to continue to move forward.
Beginning in March of this year, the American Association for Cancer Research (AACR) began hosting scientific conferences online, and last week, the AACR Virtual Meeting: Advances in Malignant Lymphoma took place. This conference, which was held in collaboration with the International Conference on Malignant Lymphoma (ICML), spanned three days and covered diverse topics, ranging from immunotherapeutic strategies to advances in single-cell analyses to health disparities in lymphoma. The meeting also incorporated real-time questions from the online audience and a virtual poster session.
“The aim of this meeting is to create a forum for brainstorming and collaboration, from bench to bedside, with extensive time devoted to exchange of ideas and lively debates on how to best achieve translation of important advances,” said meeting Chair Ari M. Melnick, MD, from Weill Cornell Medical College in New York, as he opened the conference. Highlights from sessions that discussed liquid biopsy-based approaches, targeting precursor cells, and lessons learned from epigenetic alterations in lymphoma are featured below.
Tailoring risk stratification using liquid biopsy-based approaches
One session at the meeting focused on the utilization of liquid biopsies for the real-time monitoring of lymphoma biology and clinical decision-making. The first talk in this session, delivered by David M. Kurtz, MD, PhD, from Stanford University in California, highlighted how liquid biopsies can shape personalized treatment decisions for patients with diffuse large B-cell lymphoma (DLBCL), an aggressive form of lymphoma.
As with other cancers, the stratification of patients with DLBCL into risk categories can guide treatment decisions. Kurtz explained that several risk stratification tools exist for patients with DLBCL, including the International Prognostic Index (or IPI), which estimates survival based on several risk factors; identifying the molecular “cell of origin,” which can be used to determine DLBCL subtypes; or measuring a patient’s response during treatment using positron emission tomography (PET), referred to as interim PET. “Largely, each of these tools provides only a fixed snapshot in time, looking at one risk factor, rather than a dynamic estimate of likely outcomes as more information is obtained over time,” Kurtz explained.
Liquid biopsies, on the other hand, can monitor tumor dynamics throughout the course of the disease by serially measuring circulating tumor DNA (ctDNA) during treatment. In addition to dividing patients into risk categories, such an approach can also determine the probability of likely outcomes for individual patients by incorporating new data as it becomes available, Kurtz said.
With this goal in mind, Kurtz and colleagues developed a risk model called CIRI, or the Continuous Individualized Risk Index. As described in their paper published in Cell, CIRI combines liquid biopsy assessments with established prognostic factors to provide real-time probability of patient survival by integrating risk assessments throughout a patient’s treatment course. This risk tool incorporates pretreatment risk factors (such as IPI, ctDNA burden, and DLBCL subtype) and interim risk factors during treatment (including interim imaging and ctDNA burden). In a cohort of 132 patients with DLBCL, CIRI outperformed each individual model for the prediction of event-free survival at 24 months and could robustly stratify patients into three risk categories, explained Kurtz.
In addition to their ability to quantitatively assess disease burden or risk estimation, Kurtz noted that liquid biopsy-based approaches can be used qualitatively to identify driver mutations and mechanisms of treatment resistance, including the emergence of mutations following therapy. He concluded his talk by noting that a critical and ongoing challenge in the field is the standardization of ctDNA measurements across multiple centers.
Targeting precursor cells to combat follicular lymphoma
Can we find and destroy lymphoma precursor cells? This question was the focus of another session at the meeting, and Jessica Okosun, MB BChir, PhD, from Barts Cancer Institute and Queen Mary University of London, talked about how genomic information can help shape our understanding of lymphomagenesis and lymphoma recurrence.

Okosun began by speaking about the notion of “lymphoma reservoirs,” or a precursor population of cells that can later lead to the development of lymphoma. Evidence for these reservoirs included a pair of cases of donor-derived lymphoma, where both the donor and the recipient of a hematopoietic stem cell transplant developed follicular lymphoma (FL) several years after transplant. In both of these cases, which have been described in Blood and in the AACR journal Cancer Discovery, the tumors from the donor and recipient were found to be clonally related, as evidenced by identical chromosomal translation, shared IGH gene rearrangements, and shared mutations.
“All of these incidences of donor-derived lymphomas have allowed us, over the years, to hypothesize that a founder population must have been seeded at the time of the transplant, providing clues that this precursor can exist many years before the development of FL,” Okosun said.
To identify additional evidence for follicular lymphoma reservoir populations, researchers have looked at patients’ tumors temporally (where tumors from multiple disease timepoints are analyzed) and spatially (where tumors from different sites of disease are analyzed). In both types of genetic analyses, tumors were found to share a common genetic ancestor, often referred to as a common progenitor cell (CPC).
“Why are we not curing FL?” Okosun posed. While therapeutic strategies effectively destroy the bulk of the tumor, a residual, cancer-repopulating reservoir is left behind, she said. “This population is probably one that we need to be focusing on,” Okosun continued. “If we knew the genetic fingerprint of the CPC, we could focus our efforts on targeting these aberrations, which might reduce the risk of relapse.”
Rather than analyzing follicular lymphoma tumors when they are at their most genetically diverse—at diagnosis, at relapse, at transformation—Okosun suggested that a better way to learn about the CPC is when the tumor is less genetically diverse, such as during pre-malignancy or during clinical remission with detectable minimal residual disease. Okosun and colleagues are beginning to construct detailed, comparative molecular maps across different disease states to better understand the reservoir population.
Understanding the lymphoma epigenome to shape treatment strategies
Another session during the meeting highlighted recent epigenetics research in the field of lymphoma. Michael R. Green, PhD, from The University of Texas MD Anderson Cancer Center in Houston, talked about the epigenetic regulator CREBBP, which encodes a histone acetyltransferase and is therefore involved in transcriptional activation.

Mutations to the CREBBP gene are common in B-cell lymphomas, and roughly two-thirds of FL tumors harbor CREBBP mutations. Further, CREBBP mutations almost invariably occur as early events and can be traced back to the CPC, Green explained. “To us, this suggests that they may be attractive therapeutic targets to investigate,” he said.
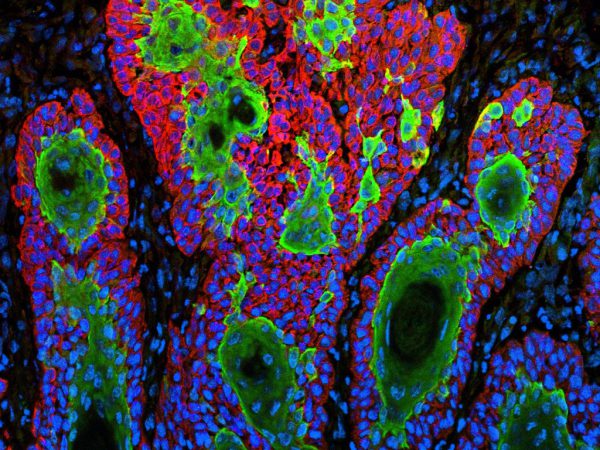
Green reviewed his study published in 2015 that demonstrated that B cells from FL tumors with CREBBP mutations had significantly lower MHC class II transcript and protein expression levels compared with FL tumors without CREBBP mutations. Analysis of T cells infiltrating CREBBP-mutant tumors revealed transcriptional signatures of decreased T-cell proliferation, suggesting that the decrease in MHC class II expression caused by CREBBP mutations results in lower levels of T-cell stimulation.
To understand how specific CREBBP mutations disrupt the epigenome, Green and colleagues used CRISPR/Cas9-mediated gene editing to introduce a common mutation in the lysine acetyltransferase domain of CREBBP into a lymphoma B cell line. This point mutation, which results in the substitution of cysteine for arginine at residue 1446 (R1446C), reduces the catalytic activity of CREBBP. The researchers found that similar regions of the genome had reduced acetylation patterns in CREBBP-mutant and CREBBP-knockout cells, yet the changes were dramatically enhanced in the CREBBP-mutant cells, including in the acetylation of the MHC class II locus. These results suggest that the CREBBP R1446C mutation may dominantly repress histone acetylation, resulting in a more severe phenotype.
To study whether these findings correlated with patient data, the researchers evaluated the outcomes of over 200 patients with follicular lymphoma according to their CREBBP mutations. They found that patients with nonsense/frameshift mutations that create a loss of protein had better survival outcomes compared with patients with point mutations in the lysine acetyltransferase domain.
To close out his talk, Green noted that patients’ tumors are typically categorized as being either CREBBP-wild type or CREBBP-mutant, but this classification system may be too simplistic. Instead, Green noted, the spectrum of CREBBP mutations could be categorized based on their effects on protein function, as the catalytic inactivity of CREBBP may dictate disease severity in patients with lymphoma.
Stay tuned
Additional topics covered at this meeting include advances in chimeric antigen receptor (CAR) T-cell therapy, how aberrant metabolism fuels lymphoma, understanding and targeting aberrant receptor signaling in lymphoma, and more. For additional coverage of this conference, keep reading Cancer Research Catalyst.