Aiming at Two Protein Targets to Treat Liver Cancer
The FDA approved a combination of an immunotherapy and a therapeutic that can stop tumors from growing blood vessels for certain patients with liver cancer.
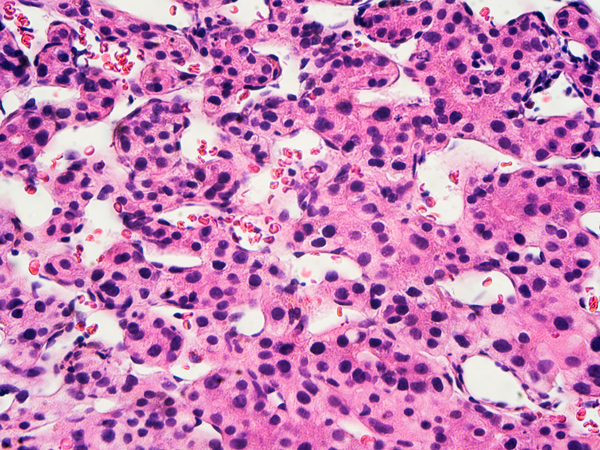
The U.S. Food and Drug Administration (FDA) approved using a combination of the immune checkpoint inhibitor atezolizumab (Tecentriq) and bevacizumab (Avastin), an agent that inhibits the process by which tumors grow blood vessels, to treat hepatocellular carcinoma, the most common form of liver cancer. The combination is indicated for patients with unresectable or metastatic hepatocellular carcinoma who have not received prior systemic therapy.
Atezolizumab and bevacizumab are both monoclonal antibodies, which are man-made versions of immune system proteins that are designed to attach to a specific target. Atezolizumab is an immune checkpoint inhibitor that hinders the function of a protein known as PD-1 to enable certain immune cells to detect and attack the cancer. Bevacizumab is known as an angiogenesis inhibitor, as it helps starve a tumor by disrupting the process of new blood vessel growth calledangiogenesis.
The approval was based upon data compiled in a multicenter, international, open-label, randomized trial. The study involved 501 patients who were randomized to receive the combination of the two monoclonal antibodies or to a second group that received sorafenib, which is another agent that stops blood vessel growth. The main efficacy outcome measures were overall survival and progression-free survival. The median overall survival was not reached in the patients who received atezolizumab plus bevacizumab and was 13.2 months in the patients who received sorafenib. The estimated average time of progression-free survival was 6.8 months for patients in the combination therapy group versus 4.3 months for those in the sorafenib arm of the study.
Hepatocellular carcinoma is the most common form of liver cancer in adults and is the leading cause of death among people with cirrhosis. It is considered a primary cancer because it starts in the liver rather than spreading to the liver from another organ. According to federal statistics, the incidence and death rates for liver cancer have been steadily rising in the United States in recent years. In 2020, there will be more than 42,000 new cases of liver cancer diagnosed and over 30,000 deaths from the disease.
The FDA approved the combination therapy on May 29, 2020.
