Editors’ Picks: December Highlights from the AACR Journals
As the year draws to a close, we bring you the final edition of Editors’ Picks for 2020. This monthly roundup features one “must read” article, handpicked by the editors, from each journal issue published by the AACR. Studies highlighted in this post include a review article about CAR T-cell therapy for the treatment of triple-negative breast cancer, a look at COVID-19-preventive behaviors among cancer survivors, and results from two clinical trials, among others. As always, articles featured here are freely available for a limited time.
Journal: Cancer Research (December 1 issue)

Loss of the NF1 protein drives aberrant activation of the RAS/MEK/ERK signaling pathway in most malignant peripheral nerve sheath tumors (MPNST), a type of soft tissue sarcoma. However, inhibitors of proteins within this pathway, including inhibitors of MEK, have shown limited efficacy for treating MPNST in preclinical or clinical studies. In this study, the authors conducted an unbiased screen to characterize the signaling changes that occur in MPNST cell lines in response to MEK inhibition. They determined that inhibition of MEK led to global activation of upstream receptor tyrosine kinases that could activate RAS signaling, thereby revealing a negative feedback loop that limits the sensitivity of the MEK inhibitor in these cells. Inhibiting the protein tyrosine phosphatase protein SHP2, which mediates RAS signaling downstream of the receptor tyrosine kinases, inactivated RAS signaling, even in MPNST cells that had acquired resistance to MEK inhibitors. The authors propose SHP2 inhibition as a potential therapeutic strategy to treat NF1-depleted MPNST. This article was featured on the cover of the December issue.
Journal: Molecular Cancer Research
Distinct Genomic Alterations in Prostate Tumors Derived from African American Men
Prostate cancer incidence and mortality are highest among African American men, but the underlying reasons for this disparity remain unclear. In this study, the authors sequenced prostate tumors from African American and white men to determine if they harbored different genetic changes. The authors found that over 35 percent of prostate tumors from African American patients harbored potentially damaging mutations in several DNA repair genes. Mutations in the DNA repair gene ZMYM3 were found in 11.7 percent of prostate tumors from African American patients, compared with 2.7 percent of tumors from white patients whose data were included in the Genomic Data Commons database. By pooling data from several public databases, the authors found that high-grade prostate tumors from African American patients were more likely to have additional copies of the MYC oncogene and deletions of several other genes, including MAP3K7 and RB1. Gain of MYC and loss of MAP3K7 or RB1 were associated with more advanced tumor stage. “Our findings suggest that distinct genetic alterations in the prostate cancers of African American men, in comparison to white men, may contribute to more aggressive prostate cancer and could lead to a higher mortality rate,” said senior author Jianfeng Xu, DrPH, in an AACR press release. This article was highlighted in the December issue.
Journal: Molecular Cancer Therapeutics
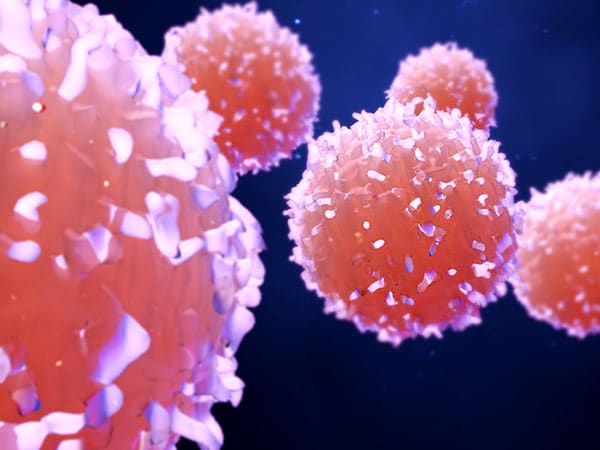
Emerging CAR-T Cell Therapy for the Treatment of Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC) is a highly aggressive disease with limited therapeutic options. Treatment with immunotherapy has recently come to the fore, as evidenced by the recent approval by the U.S. Food and Drug Administration (FDA) of the checkpoint inhibitor pembrolizumab (Keytruda) for locally recurrent unresectable or metastatic TNBC. Another type of immunotherapy, chimeric antigen receptor (CAR) T-cell therapy, is currently being investigated in solid tumors, including TNBC. This review highlights the challenges of CAR T-cell therapy in solid tumors, such as target antigen heterogeneity/lack of target antigen specificity, an immunosuppressive tumor microenvironment, and poor persistence, with examples of mitigation strategies in TNBC. The article also focuses on promising targets for CAR T-cell therapy in TNBC, including the cell surface glycoproteins mesothelin and MUC1, the receptor tyrosine kinases AXL and c-Met, and the stress ligand NKG2D, referencing key preclinical results. Finally, the authors describe multiple phase I clinical trials of CAR T-cell therapy for the treatment of TNBC. This article is highlighted in the December issue.
Journal: Cancer Prevention Research
Prostate cancer is the leading cause of cancer-related death among men in the United States. Given the delayed onset and slower progression of prostate cancer compared to other cancer types, the identification of chemoprevention methods is of great interest. The histone methyltransferase EZH2 is overexpressed in high-grade prostatic intraepithelial neoplasia (HG-PIN)—a precursor of prostate cancer—and has been implicated in prostate cancer initiation and recurrence, providing a potential target for chemoprevention. In this study, the authors used mouse and cell line models of HG-PIN and MYC-driven prostate cancer to determine the impact of EZH2 inhibition. They found that inhibiting EZH2 activity by genetic manipulation or with a chemical inhibitor reversed the HG-PIN phenotype, decreased the overall weight of the genitourinary tract and prostate, reduced cellular proliferation, and induced p53-dependent cellular senescence. The authors propose EZH2 inhibition as a potential chemoprevention approach for prostate cancer. This article was featured on the cover of the December issue.
Journal: Cancer Epidemiology, Prevention & Biomarkers
The COVID-19 Impact Survey aims to provide national and regional statistics about physical health, mental health, economic security, and social dynamics in the United States during the COVID-19 pandemic. In this study, the authors merged data from three weeks (April 20-26, May 4-10, and May 30-June 8) and evaluated COVID-19-related preventative behaviors of 10,760 adults, 854 (7.6 percent) of whom self-reported a diagnosis of cancer (defined as cancer survivors). Compared with those without cancer, cancer survivors were more likely to practice social distancing, wear a face mask, and avoid crowded areas. While cancer survivors were less likely to cancel social activities, such as work and school-related activities, they were more likely to cancel doctor’s appointments, compared with adults without cancer. When the researchers accounted for covariates, they found that non-Hispanic Black cancer survivors were less likely to cancel a doctor’s appointment compared with non-Hispanic white cancer survivors. Further, cancer survivors who were young adults (ages 18-29), female, or who had at least one comorbid condition were more likely to cancel a doctor’s appointment. The authors note that the continuity of care for cancer survivors may be disrupted by the COVID-19 pandemic, with specific populations being most impacted. This article was highlighted in the December issue.
Journal: Cancer Immunology Research
Immune Remodeling of the Extracellular Matrix Drives Loss of Cancer Stem Cells and Tumor Rejection
The tumor microenvironment (TME) has been shown to influence the response to cancer immunotherapy. The authors of this study previously showed that depletion of immunosuppressive regulatory T (Treg) cells in a mouse model of fibrosarcoma led to control of tumor growth; however, this response was only seen in about 50 percent of mice. In the latest study, the authors examined whether differences in the TME might contribute to the variability in the responses to Treg depletion. Using the same mouse model, they compared the TMEs of Treg-depleted responders with those of Treg-depleted non-responders. They found that the TMEs of responding tumors were enriched with T cells and had low expression of several extracellular matrix proteins, while the converse was true for non-responding tumors. Responding tumors also had distinct lymphatic and blood vessel networks. Ectopic expression of an extracellular matrix protein prior to Treg depletion did not hinder the establishment of an antitumor response, suggesting that changes to the extracellular matrix are likely a consequence, and not the underlying cause, of an antitumor immune response. The authors propose that the immune response not only targets cancer cells but may also contribute to the remodeling of the TME by promoting the loss of ECM proteins. This article was featured on the cover of the December issue.
Journal: Cancer Discovery
Patients with localized non-small cell lung cancer (NSCLC) typically receive radiation therapy; however, approximately 30 percent of patients experience local recurrence after treatment. In this study, the researchers sequenced tumors of 232 patients with localized NSCLC to identify associations between tumor genotype and outcomes after radiation. They found that approximately half of local recurrences occurred in patients whose tumors had mutations in the transcription-regulating genes KEAP1 and NFE2L2. Loss-of-function mutations in KEAP1 and gain-of-function mutations in NFE2L2 were associated with increased radioresistance. Since KEAP1-mutant cells have been shown to be dependent on glutamine metabolism, the authors explored whether inhibiting glutamine metabolism might sensitize KEAP1/NFE2L2-mutated cells to radiation. Compared with untreated cells, KEAP1/NFE2L2-mutated cell lines treated with a small molecular inhibitor of glutaminase were significantly more sensitive to ionizing radiation due to increased levels of reactive oxygen species and greater DNA damage. The authors conclude that mutations in KEAP1 and NFE2L2 could function as biomarkers to predict outcomes after radiation therapy and propose targeting glutamine metabolism as a potential strategy to radiosensitize KEAP1/NFE2L2-mutated NSCLC. This article was highlighted and featured on the cover of the December issue.
Journal: Clinical Cancer Research (December 1 issue)
In addition to targeting the tumor, targeting the TME is an attractive strategy for the treatment of children with refractory cancer. Pexidartinib (Turalio), which has been approved for the treatment of adult patients with tenosynovial giant cell tumor, inhibits class III tyrosine kinases, such as colony-stimulating factor 1 receptor (CSF-1R). CSF-1R signaling is important for many functions of immunosuppressive myeloid cells, such as mobilization, migration, survival, and proliferation, suggesting that pexidartinib may impact the TME. In this phase I clinical trial, pexidartinib was evaluated in 16 children/young adults with refractory leukemias or solid tumors (median age was 16 years). No dose-limiting toxicities were observed, and the recommended phase 2 dose (RP2D) was determined to be weight-based. Two patients had stable disease, and one patient with peritoneal mesothelioma had a sustained partial response. The authors note that pexidartinib is being investigated in adult clinical trials and warrants further investigation in the pediatric population. This article was highlighted in the December 1 issue.
Journal: Cancer Research (December 15 issue)

Peritoneal seeding of malignant cells facilitates ovarian cancer metastasis, with the survival of non-adherent ovarian cancer cells in the peritoneal fluid and their later adherence to the mesothelium of distant organs leading to cancer progression. However, the underlying mechanisms of these processes have not been fully elucidated. To better understand factors that facilitate tumor cell survival and proliferation, the study authors cultured ovarian cancer cells in both adherent and non-adherent conditions and analyzed changes in mRNA and protein levels. They found that the EGFR pathway is critical for the survival of non-adherent cells and that the transcription factor FOXM1 regulates integrins and matrix proteins that mediate the adhesion of cancer cells and their subsequent colonization. Combinatorial treatment of ovarian cancer cells with the EGFR inhibitor lapatinib and the FOXM1 inhibitor thiostrepton reduced growth and peritoneal spread more effectively than either drug alone. The authors conclude that the EGFR and FOXM1 pathways may be viable targets to disrupt ovarian cancer metastasis. This article was featured on the cover and was highlighted in the December 15 issue.
Journal: Clinical Cancer Research (December 15 issue)
While treatment with endocrine therapy plus a CDK inhibitor is efficacious in some postmenopausal patients with hormone receptor (HR)-positive, HER2-negative advanced breast cancer, most patients eventually experience disease progression due to endocrine resistance. Preclinical research indicates that inhibition of the PI3K pathway could potentially overcome endocrine resistance. In this phase Ib clinical trial, the triplet combination of the CDK inhibitor ribociclib (Kisquali), the mTOR inhibitor everolimus (Afinitor/Zortress), and the aromatase inhibitor exemestane (Aromasin) was evaluated in 116 patients with HR-positive, HER2-negative, pretreated advanced breast cancer. Of these patients, 83 were enrolled in the dose-escalation phase, and 33 were enrolled in the dose-expansion phase. The RP2D was determined to be 25mg daily of exemestane, 2.5mg daily of everolimus, and 300mg of ribociclib, taken daily with food for three weeks on/one week off in a four-week cycle. Treatment was generally well-tolerated, and the safety profile was consistent with the known profiles of the combination partners. Preliminary evidence of antitumor activity was observed, and higher expression of the ESR1 gene trended with better response to the triplet therapy. The authors note that further biomarker investigation is warranted to help identify patients that could most benefit from this combinatorial treatment. This article was highlighted in the December 15 issue.