Groundbreaking New Immunotherapy Approved for Acute Lymphoblastic Leukemia (ALL)
The U.S. Food and Drug Administration has approved the first of a new type of immunotherapy called CAR T-cell therapy for ALL.
We recently reached a highly anticipated milestone for the oncology community when the U.S. Food and Drug Administration (FDA) announced the first approval of a type of immunotherapy known as CAR T-cell therapy.
The approved CAR T-cell therapy is called tisagenlecleucel (Kymriah). Known through most of its development as CTL019, tisagenlecleucel was approved for treating certain pediatric and young adult patients with acute lymphoblastic leukemia (ALL).
Tisagenlecleucel is intended for children and young adults up to the age of 25 with B-cell ALL that is refractory, meaning that it has not responded to standard treatments, or has relapsed at least twice.
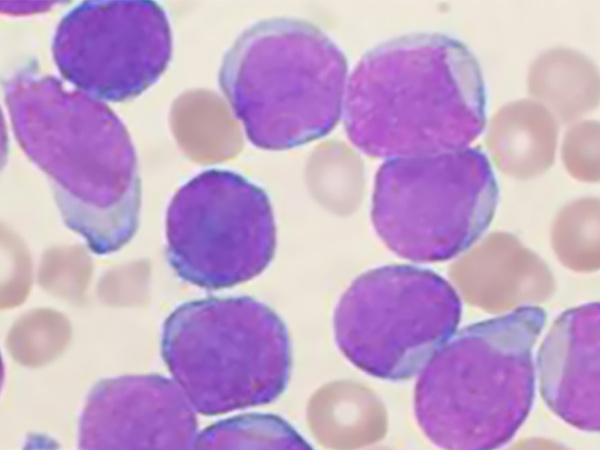
ALL is the most common cancer diagnosed in children, according to the National Cancer Institute. Substantial progress has been made in treating children with ALL; about 85 percent of those diagnosed between the ages of 1 and 18 who receive the current standard treatments are expected to have long-term survival without disease relapse. However, outcomes for those whose leukemia is refractory to treatment or relapses are poor.
Most ALL cases in children are classified as B-cell ALL, which means the leukemia originated in immune cells called B cells. B-cell ALL cells almost always have a protein called CD19 on their surface, making it an attractive therapeutic target.
Tisagenlecleucel is a cell-based therapy that targets CD19-positive cells. Each patient receives a customized dose of tisagenlecleucel that is created using immune cells called T cells harvested from his or her blood. Once the T cells have been harvested, they are genetically modified to have a new gene that encodes a protein called a chimeric antigen receptor (CAR). After the T cells are modified, they are expanded in number and then infused back into the patient. The CAR directs the infused modified T cells to CD19-positive B cell ALL cells and triggers them to attack once they get there.
The approval of tisagenlecleucel was based on results from the phase II ELIANA clinical trial. According to the FDA, 83 percent of the 63 children and young adults who were treated with tisagenlecleucel had remission within three months of receiving the CAR T-cell therapy. Previously published data from earlier, smaller clinical trials suggest that for some patients, remission following tisagenlecleucel treatment is durable, but further follow-up is needed to determine long-term overall survival rates.
It is important to note, however, that treatment with tisagenlecleucel can cause severe adverse effects. One of the most concerning of these is cytokine-release syndrome, which is a systemic response to the activation and proliferation of the CAR T cells that causes high fever and flu-like symptoms. It can also cause life-threatening neurological events. Thus, the approval comes with a boxed warning for cytokine-release syndrome and neurological toxicities. In addition, the FDA expanded the approval of a medication called tocilizumab (Actemra) to include the treatment of CAR T cell-induced severe or life-threatening cytokine-release syndrome in patients ages 2 and older. This expanded approval was based on clinical trial data showing that 69 percent of patients treated with CAR T-cells had complete resolution of cytokine-release syndrome within two weeks following one or two doses of tocilizumab.
To further reduce risk to patients receiving tisagenlecleucel, the FDA has put in place a risk evaluation and mitigation strategy that requires that health care facilities using the new treatment be specially certified. As part of that certification, the health care facilities must have onsite, immediate access to tocilizumab and the staff involved in the prescribing, dispensing, or administering of tisagenlecleucel must be trained to recognize and manage cytokine-release syndrome and neurologic events.
Despite the risks associated with tisagenlecleucel treatment, the future looks bright for the groundbreaking new approach to cancer treatment. For example, early results suggest that tisagenlecleucel shows promise as a treatment for adults who have diffuse large B-cell lymphoma that is refractory to standard treatments or has relapsed after two or more prior therapies, and the FDA granted breakthrough therapy designation to the immunotherapeutic for this use.
Other CD19-targeted CAR T-cell therapies are also under development.
The FDA approval was rendered on August 30, 2017.
