Biosimilars: Breaking Through to Cancer Treatment
A little-talked-about provision of the 2010 Patient Protection and Affordable Care Act designed to improve access to innovative medical therapies has recently borne fruit for the cancer community in the form of two new therapeutic options for a wide range of cancers—bevacizumab-awwb (Mvasi) and trastuzumab-dkst (Ogivri).

The FDA recently approved two anticancer therapeutic biosimilars, bevacizumab-awwb (Mvasi) and trastuzumab-dkst (Ogivri).
The provision in question amended the Public Health Service Act to “allow a person to submit an application for licensure of a biological product based on its similarity to a licensed biological product.” In simple terms, it led to the U.S. Food and Drug Administration (FDA) establishing a shortened path for approving therapeutics known as biological products that have been shown to be “highly similar” (biosimilar) to biological products already approved by the agency.
But what are biological products and biosimilars, and what might the emergence of biosimilars mean for cancer treatment moving forward?
Biological products and biosimilars 101
Most anticancer therapeutics, in particular the chemotherapeutics that have been the mainstay of cancer care for decades and many of the molecularly targeted therapeutics that form the backbone of precision cancer medicine, have well-defined chemical structures and are made by combining specific chemical ingredients in an ordered manufacturing process.
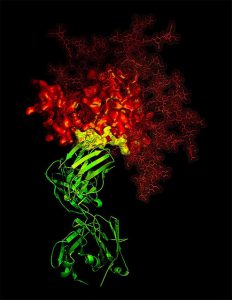
Antibody B12. Monoclonal antibodies are used to treat a wide array of types of cancer. Image courtesy of the National Cancer Institute.
Over the years, advances in biotechnology have led to the emergence of a different category of anticancer therapeutics known as biological products. The term can encompass a wide array of products isolated from natural sources such as humans, animals, and microorganisms. Currently, most FDA-approved biological anticancer therapeutics are large, complex molecules known as monoclonal antibodies. Examples of monoclonal antibodies used in cancer care include trastuzumab (Herceptin), which is primarily used to treat patients with HER2-positive breast cancer, and the checkpoint inhibitors atezolizumab (Tecentriq), avelumab (Bavencio), durvalumab (Imfinzi), nivolumab (Opdivo), and pembrolizumab (Keytruda), which are used to treat an increasing number of types of cancer.
Biosimilars are biological products that the FDA deems are highly similar to and have no clinically meaningful differences from existing FDA-approved biological products, known as reference products. In practice, this means the FDA has determined that data comparing a biosimilar and reference product—for example, trastuzumab-dkst and trastuzumab—show that certain characteristics, including purity, molecular structure, and bioactivity, are highly similar and that there are no clinically meaningful differences in safety and effectiveness. Importantly, because the requirement is to demonstrate biosimilarity, and not to independently establish the safety and effectiveness of a proposed biosimilar product, expensive and lengthy large-scale clinical trials are usually not required.
Even though the concept of biosimilars is like that of generic drugs—alternative versions of brand-name therapeutics—they are not the same. Generic drugs are developed by chemically synthesizing exact copies of the active ingredients of brand-name drugs. But because biosimilars are developed using complex living systems, they are usually slightly different from the reference biological product. Given the differences, the development of generic drugs and biosimilars are governed by different legislation and they are approved through different regulatory paths.
Biosimilars and cancer treatment
According to the FDA, biological products are the fastest-growing class of therapeutics in the United States. In oncology, the number of new biological anticancer therapeutics has been increasing steadily over the past decade. Thus far in 2017, there have been five new biological anticancer therapeutics approved, including two of a revolutionary new type of cancer treatment called CAR T–cell therapy.
Given the growing importance of biological anticancer therapeutics in the care of patients with cancer, the emergence of biosimilars will provide more treatment options for oncologists and their patients. As FDA Commissioner Scott Gottlieb, MD, outlined recently, the hope is also that “Biosimilars can potentially reduce costs for consumers by creating price competition for products that previously faced few market competitors.” In theory, reduced costs will improve access and promote better public health outcomes.
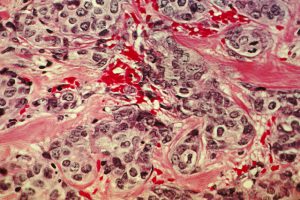
Breast cancer cells. Breast cancer is one of the types of cancer for which a biosimilar has been approved by the FDA. Image courtesy of the National Cancer Institute.
Overall, the number of FDA-approved biosimilars has more than doubled in 2017, increasing from four approved biosimilars at the start of the year to nine, as of Dec. 12, 2017. Two of the most recent approvals are anticancer therapeutics. Bevacizumab-awwb is a biosimilar of bevacizumab (Avastin) and it was approved in September 2017 by the FDA for most of the uses for which bevacizumab has been approved—treatment of certain adult patients with cervical, colorectal, kidney, and lung cancers, and certain patients with glioblastoma. More recently, on December 1, 2017, a biosimilar of trastuzumab (Herceptin) called trastuzumab-dkst was approved for treating certain patients with HER2-positive breast or metastatic stomach cancer, approvals granted in previous years for trastuzumab.
Given that these biosimilars have only recently been approved, it is not yet clear how widely they will be used compared with the brand-name equivalents and whether they will in fact achieve the goal of improving access to treatment. To address this issue, the FDA recently announced it was launching an educational campaign to ensure that health care providers fully understand what biosimilars are, and how they can help patients.