SABCS 2022: Panelists Discuss Strategies to Overcome Top Obstacles in Breast Cancer Management
Researchers, physicians, patients, and other stakeholders convened in San Antonio, Texas, December 6-10 for the annual San Antonio Breast Cancer Symposium (co-sponsored by the AACR), where exciting new advances in clinical and basic breast cancer research were disseminated.

Coupled with the buzz surrounding the strides in breast cancer research was the acknowledgement that various barriers and gaps in knowledge continue to limit progress. To shed light on these obstacles, 10 experts from the realms of breast cancer research, clinical management, and patient advocacy came together for a panel discussion titled “Overcoming the Big Obstacles to Find Solutions for Breast Cancer.”
The two-hour discussion was moderated by Carlos Arteaga, MD, FAACR, SABCS co-director, a Past President of the AACR, and director of the Simmons Comprehensive Cancer Center; and Angela DeMichele, MD, MSCE, an oncologist and professor at the University of Pennsylvania Perelman School of Medicine.
During this session, panelists and audience members identified some of the top obstacles facing the breast cancer field and proposed innovative strategies to surmount them.
Obstacle #1: The Need for Targeted Prevention, Early Detection, and Interception
According to panelist Christine Ambrosone, PhD, “prevention of breast cancer at the population level is unlikely” due to the plethora of risk factors and the heterogeneity of the disease. Therefore, she argued that the priority should be the prevention and interception of the high-risk, aggressive breast cancers that are most likely to cause death. At the same time, she said, it will be important to minimize the overdiagnosis and treatment of low-risk breast cancers that are unlikely to cause significant morbidity or mortality. To this end, she believes polygenic risk scores will be a valuable tool to identify patients with the greatest risk of lethal breast cancer.

Panelist Joan Brugge, PhD, FAACR, identified interception as the top priority to reducing breast cancer mortality. To improve interception, she argued, we need better biomarkers to recognize the premalignant lesions that are likely to progress, which will require a deeper understanding of how the tumor microenvironment influences progression to invasive breast cancer. In addition, screening and diagnostic tools with enhanced sensitivity are needed to detect premalignant cells at the earliest stages of development, and effective interventions are needed to prevent their progression.
Additional strategies discussed by the panelists and audience members included initiating genetic screening at earlier ages, exploring the prophylactic potential of PARP inhibitors, and encouraging healthier lifestyles.
Obstacle #2: Underutilization of Artificial Intelligence, Big Data, and Digital Transformation
Panelists Regina Barzilay, PhD, and Yeon Hee Park, MD, PhD, advocated for increased use of artificial intelligence, big data, and digital transformation in breast cancer management. The top priority for Barzilay is utilizing these tools to better tailor treatment to each individual patient. Stratifying patients based on biomarkers in their breast cancers would be one approach, but the underutilization of retrospective clinical trial data has impeded progress on this front. In the United States, the lack of a centralized medical database limits access to such data; in other countries, strict privacy regulations are an obstacle.
Panelists and audience members identified several obstacles to implementing artificial intelligence in the clinic. One issue is that most members of the workforce are not trained in this technology. Another issue is that the lack of a centralized medical database has resulted in insufficient data to develop artificial intelligence algorithms for breast cancer.
Park argued that increasing the use of digital tools, such as electronic data transfer and remote patient monitoring, would improve treatment and increase accessibility to clinical trials. She advocated for the loosening of various bureaucratic and regulatory barriers that currently impede the use of these tools.
Obstacle #3: Slow Implementation of Precision Medicine
Fabrice André, MD, PhD, contended that the current system of evaluating and approving treatments by cancer type is limiting the reach of precision medicine. Instead of this approach, he broached the idea of categorizing tumors by their molecular features and potentially extending the approval of a molecularly targeted therapy that is effective in one cancer type to other types fueled by the same molecular driver. In addition, investing in the development of molecular testing tools would improve the identification of tumors that would respond to certain treatments.
Matthew Ellis, MD, PhD, explained that one of the issues with precision medicine research is that molecular features are not studied within the context of their intracellular and extracellular environments. Studying the impacts of post-translational modifications and the tumor microenvironment, among other factors, will be critical to identifying appropriate therapeutic targets.
Obstacle #4: Bureaucratic Challenges and the Lack of Diversity in Clinical Trials
Randomized clinical trials are considered the gold standard for evaluating new therapies, but Nadia Harbeck, MD, PhD, made the point that they are not always feasible or even scientifically appropriate. Therefore, she believes that the field needs to implement more real-world evidence in order to expedite the evaluation of experimental therapies.
An audience member added that the current standards for data quality in clinical trials are prohibitively high. She noted that easing the stringent standards to more closely match the requirements of real-world data could make conducting randomized clinical trials easier and less costly.
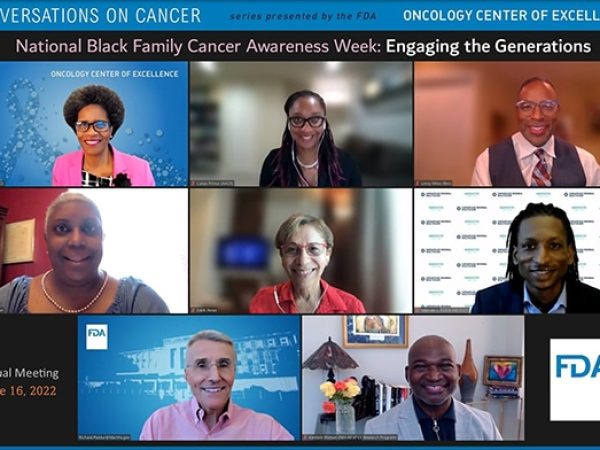
For Eric Winer, MD, the top priority for revamping clinical trials is to increase their diversity—both in the racial makeup of the patient population and the tumor stages included. This would allow clinicians to better understand the efficacies of new therapies in minority patients (who may be more likely to die from their breast cancers) and in various disease contexts.
Obstacle #5: Disparities in Patient Outcomes
The first step to reducing cancer health disparities is to acknowledge that racism exists, said Lori Pierce, MD. Only then, she added, can we mitigate our own implicit biases and identify the changes needed to improve outcomes for all patients. She encouraged clinicians to listen to their patients better and understand the systemic and personal barriers that they may face. In addition, she advocated for talking to patients, particularly those from underserved backgrounds, about making lifestyle changes that could reduce cancer risk.
Patient advocate Patty Spears, BS, identified access to clinical trials as a major barrier. She proposed broadening eligibility criteria to make clinical trials available to more patients, especially men; decentralizing trials so patients can receive care closer to their homes; and engaging patient navigators from diverse backgrounds to help patients through the complicated health care system in a culturally sensitive manner.
Obstacle #6: Limited Research Funds and the “Academic Brain Drain”
The final portion of the discussion, which centered on improving the research climate, included perspectives from André, Brugge, and Pierce.
To make the greatest impact, André believes that more research funds should be allocated to solution-based, interdisciplinary projects with the greatest potential to advance the field. He added that funding should be large enough to support not only the research but also a reasonable quality of life for researchers.
Brugge and Pierce identified changes needed to limit the “academic brain drain” that is causing researchers to leave academia for industry positions. Both argued for enhancing the quality of life for academic researchers: Brugge noted that higher salaries and larger research grants are needed, and Pierce advocated for family-friendly policies to improve work-life balance. In addition, Pierce said that in today’s funding climate, junior researchers need more time to secure funding before applying for tenure. She added that the elusive R01 grant should be deprioritized in promotions, and collaboration and entrepreneurship should be rewarded.
Implementation of the strategies proposed here could potentially address many of the complex issues facing breast cancer research and clinical care, and may ultimately help expand the reach of research breakthroughs to more patients.