Pausing Breast Cancer Treatment to Get Pregnant, and Other News from SABCS 2022
Amy Bianchi discovered a lump in her breast when her first child was 18 months old. She was diagnosed with cancer, and after surgery, began taking endocrine therapy to reduce the risk of recurrence.
She was happy to be free of cancer, but dreamed of another baby. Pregnancy is not recommended for women taking endocrine therapy, due to potential risks to the developing fetuses. But Bianchi heard about a scientific study in which women could take a break from their endocrine therapy to try and get pregnant. She decided to enroll.
Today, Bianchi is a healthy mother of two. She gave birth to son Brayden, nursed him for six months, then resumed her endocrine therapy.
Bianchi was part of the international POSITIVE clinical trial, which enrolled 518 women between December 2014 and December 2019 and followed them as they paused their endocrine therapy and tried to conceive. They monitored the women to evaluate their risk of recurrence. After 41 months of follow-up, 8.9 percent of the women had experienced a recurrence, compared with 9.2 percent of women in an external control cohort.
What’s more, 365 babies were born. Of 497 women followed for pregnancy status, 368 had at least one pregnancy and 317 had at least one live birth.
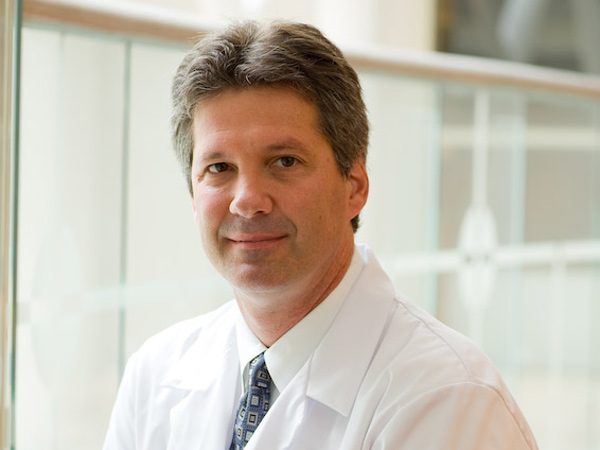
Ann Partridge, MD, MPH, vice chair of medical oncology at Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, presented results of the study at the San Antonio Breast Cancer Symposium (SABCS), held December 6-10, 2022. She cautioned that longer follow-up will be necessary to fully understand the risk of recurrence, but results to date indicate that the decision to pause therapy can be made safely, in consultation between women and their physicians.
“Pregnancy after breast cancer is a very personal decision for which, ideally, a woman should take into account not only her desire to carry a pregnancy, but her baseline fertility, prior and current treatment, and any fertility preservation strategy she may have pursued, as well as the underlying risk of cancer recurrence she faces,” said coauthor Olivia Pagani, MD, international study chair on behalf of the International Breast Cancer Study Group, in an AACR press release.
As for Bianchi, the study gave her a second chance at motherhood that doctors initially discouraged, she told The Associated Press.
“If I had listened to the first few doctors or oncologists that I spoke with, I would have lost all my hope,” she shared. “I would have very quickly accepted that I would never have the family that I had envisioned.”
The Associated Press story appeared in many national outlets, including the Los Angeles Times and The Seattle Times. The study was also covered by NBC News. [Editor’s note: In May 2023, the study was published in The New England Journal of Medicine.]
The POSITIVE study was just one of numerous stories that emerged from this year’s SABCS. The American Association for Cancer Research (AACR) is a cosponsor of the symposium, an annual gathering highlighting cutting-edge breast cancer research.
Here are a few other studies that received national and international media attention:
A new therapeutic option is extending survival for some metastatic breast cancer patients
Trastuzumab deruxtecan (T-DXd) was approved by the U.S. Food and Drug Administration (FDA) in late 2019 to treat certain patients with unresectable or metastatic HER2-positive breast cancer that progressed despite treatment with two or more other HER2-targeted treatment regimens after the diagnosis of metastatic disease.
At this year’s SABCS, Ian Krop, MD, PhD, associate cancer center director for Clinical Research and the chief clinical research officer at the Yale Cancer Center, shared results from the DESTINY-Breast02 trial, which was designed as a confirmatory study for DESTINY-Breast01, which led to the accelerated approval of T-DXd.
The new study showed that compared with chemotherapy-based regimens, T-DXd yielded higher response rates and longer survival for patients who had previously been treated with trastuzumab emtansine (T-DM1). Among the patients treated with T-DXd, 69.7 percent experienced an objective response, as compared with 29.2 percent of patients who received a chemotherapy-based treatment.
This story was covered by HealthDay and syndicated to more than 150 outlets, including U.S. News and World Report.
Adding to this encouraging news for patients with metastatic breast cancer, researchers shared results from the DESTINY-Breast03 trial that showed that second-line treatment with T-DXd led to significantly longer overall survival compared with T-DM1 in patients with HER2-positive metastatic breast cancer.
According to lead author Sara Hurvitz, a professor of medicine at the David Geffen School of Medicine at the University of California Los Angeles and Jonsson Comprehensive Cancer Center, patients treated with T-DXd had a 36 percent lower risk of death than those treated with T-DM1. Their median progression-free survival was 28.8 months, compared with 6.8 months for patients treated with T-DM1.
“These updated results do demonstrate remarkable [overall survival] and [progression-free survival] benefits, solidly placing T-DXd as the standard of care,” Hurvitz said in a press conference in San Antonio. Media outlets including STAT and Cancer Health featured this study.
Women with multiple tumors may be able to opt for less-invasive surgery
The Associated Press also covered a study that showed that women with multiple breast tumors may be able to choose lumpectomies rather than mastectomies.
Lead author Judy C. Boughey, MD, the W.H. Odell Professor of Individualized Medicine and Chair of the Division of Breast and Melanoma Surgical Oncology at the Mayo Clinic, explained that improvements in imaging technology have resulted in more women being diagnosed with multiple breast tumors. To date, most of these patients have been recommended to undergo a mastectomy, rather than breast-conserving therapy consisting of lumpectomy and radiation.
The ACOSOG Z11102 (Alliance) prospective phase II clinical trial evaluated nearly 200 women with two or three tumors in one breast who underwent lumpectomy. After five years of follow-up, their rate of recurrence was 3 percent—comparable to women who had a single tumor and underwent the same surgery.
Boughey said the study adds to a body of research that is helping identify the most appropriate treatment for each patient, rather than assigning the same treatment to all patients, which can result in overtreating some.
Phase III trial shows improved survival with addition of an AKT inhibitor
Patients with HR-positive, HER2-negative breast cancer are commonly treated in the first line with an endocrine therapy—such as an aromatase inhibitor, which blocks the production of estrogen—alongside a CDK4/6 inhibitor, which stalls the cell cycle. Eventually, however, most tumors develop resistance to these therapies, and options for further treatment are limited.
Results of the phase III CAPItello-291 clinical trial, presented by Nicholas Turner, MD, PhD, a professor of molecular oncology at The Institute of Cancer Research, London, and a consultant medical oncologist at The Royal Marsden NHS Foundation Trust, showed that adding capivastertib, an investigational AKT inhibitor, to fulvestrant doubled the mean progression-free survival to 7.2 months, compared with 3.6 months for patients who received fulvestrant plus a placebo. This study was covered by CNN.
Black women experience worse outcomes despite similar risk-prediction scores
Black women are known to experience worse outcomes from breast cancer than white women. This disparity persists across multiple breast cancer subtypes.
One study discussed at SABCS showed that attempts to predict the chance of breast cancer recurrence do not adequately capture risk for Black women. In an analysis of data from the RxPONDER clinical trial, researchers discovered that despite similar scores on a 21-gene recurrence assay, Black women with lymph node-positive, HR-positive/HER2-negative breast cancer were more likely to have high-grade tumors and lower rates of invasive disease-free survival.
After adjusting for age, menopausal status, grade, treatment arm, and recurrence score, Black patients had a 37 percent increased risk of invasive cancer compared with white patients, suggesting that biological differences are a major factor in disparate outcomes.
“There is now wide-ranging evidence for differences in tumor biology contributing to this disparity. Understanding these differences will help us discover new opportunities for intervention that will ultimately reduce cancer health disparities,” said presenter Yara Abdou, MD, assistant professor at the University of North Carolina at Chapel Hill and Lineberger Comprehensive Cancer Center. This study was covered by Healio, OncLive, and Pharmacy Times, among many other publications.
Cancer Research Catalyst will continue to report on some of the major themes from SABCS. This post covered a panel of eminent breast cancer researchers discussing ways to overcome chief obstacles in breast cancer research, and this post discussed efforts to treat patients with less intensive, therefore less toxic, therapies. Check back soon and subscribe to the blog to read additional posts.