Pancreatic Cancer: Keynote Highlights Trainees, Rising Stars, and Distinguished Professors
In the opening keynote session of the AACR Special Conference on Pancreatic Cancer, which took place September 27-30 in Boston, co-chair Jen Jen Yeh, MD, exemplified the excitement and passion exuding from the researchers in attendance.
“There is so much enthusiasm in the room,” said Yeh, a professor of surgery and pharmacology at the University of North Carolina at Chapel Hill, director of the UNC Lineberger Pancreatic Cancer Center of Excellence, and Vice Chair for Research in the Department of Surgery. “It’s really, really amazing to see this community of committed pancreatic cancer researchers and clinicians.”
This excitement was echoed by co-chair Anirban Maitra, MBBS, a professor of pathology and translational molecular pathology and Scientific Director of the Sheikh Ahmed Pancreatic Cancer Research Center at the University of Texas MD Anderson Cancer Center.
“This is a meeting for everyone who works in pancreas cancer,” Maitra said. “The idea is, in the next three-and-a-half days, you just literally get immersed in this field and understand how you can work together and make a difference.”
Yeh and Maitra, alongside co-chairs Rosalie C. Sears, PhD, a professor of molecular and medical genetics and co-director of the Brenden-Colson Center for Pancreatic Care at the Oregon Health and Science University School of Medicine; and Christine A. Iacobuzio-Donahue, MD, PhD, a pathologist and director of the center for Pancreatic Cancer Research at Memorial Sloan Kettering Cancer Center and the editor-in-chief of the AACR journal Cancer Research, designed the program to call attention to existing gaps in pancreatic cancer care and empower the record-breaking 700+ registrants to address those gaps.
“We hope all of the graduate students and postdoctoral fellows in the room who are listening to these talks … think, ‘this is a way I can impact the field,’” Maitra said.
In support of this goal, the opening keynote session showcased the ways researchers across all career stages are contributing to unmet needs in pancreatic cancer—from the keynote presentation given by Iacobuzio-Donahue, to the Rising Star Keynote delivered by an assistant professor, to a handful of “lightning talks” presented by graduate students and postdoctoral trainees.
Palm Trees or Baobabs?

Iacobuzio-Donahue studies the evolution of pancreatic cancer from a precancerous lesion to a metastatic tumor. She used an arboreal analogy to describe what she’s learned about the landscape of mutations at different stages of tumor development.
“I used to think of pancreatic cancer as a palm tree,” she explained; the long trunk represented “truncal” mutations that occurred before the tumor invaded nearby tissue, while the short branches represented “subtruncal” mutations that evolved across different parts of the tumor and its metastases.
As Iacobuzio-Donahue learned more, however, she began to think of pancreatic cancer more as a baobab tree, another tall tree with even shorter, stubbier branches and a very broad trunk.
Such analyses of truncal and subtruncal mutations were previously difficult, she explained. Sequenced samples mostly came from tissues that were surgically removed, which is typically only attempted for early-stage pancreatic tumors. Iacobuzio-Donahue and colleagues sequenced the DNA of 565 tumor samples from 90 patients with various stages of disease, most of which were collected upon autopsy. Having multiple tumor samples per patient (a median of five) allowed the researchers to decipher the evolutionary history of each patient’s disease.
They found that over 70% of the mutations driving pancreatic cancer occurred before tumor invasion, hence the broad trunk of the baobab tree. A higher truncal mutation density—more mutations per region of DNA—was associated with a significantly worse prognosis; tumors with the thickest mutational tree trunks imparted a 2.89-fold increased risk of death compared to tumors with the thinnest mutational tree trunks.
Iacobuzio-Donahue suggested that her team’s observations about truncal mutations could have clinical implications for therapies that target tumor drivers.
“They’re present in virtually all cells in the neoplasm,” she said. “I think that’s very promising as we are moving into this era of targeted therapies.”

Harnessing RNA Biology
The success of mRNA-based vaccines against COVID-19 helped to bring RNA—the genetic material that dictates when and where proteins are made—into the limelight. But Luisa Escobar-Hoyos, MSc, PhD, the Rising Star Keynote speaker and an assistant professor of therapeutic radiology at Yale School of Medicine, has been studying the complexities of RNA in pancreatic cancer for years.
Part of her journey began with the observation that many aggressive pancreatic tumors, often of the basal subtype, express keratin 17, an embryonic form of keratin that isn’t found in normal adult tissues. A closer look revealed the expression of other embryonic genes that suggested the presence of an RNA “switch” differentiating the highly aggressive tumors from other tumors.
Escobar-Hoyos began looking for other such switches and studied what caused them.
“As I started looking more at the transcriptional profiles of these subtypes, I realized that the basal molecular subtype had, also, a transcriptional signature of increased RNA splicing proteins, suggesting that, potentially, not only was RNA expression important in these aggressive tumors, but also RNA processing—in particular the RNA splicing,” Escobar-Hoyos said.
RNA splicing is a crucial step in RNA processing that removes unnecessary regions of RNA before it is translated into a protein. Some pieces of RNA, called cassette exons, can be included in or excluded from the final transcript depending on physiological conditions. Escobar-Hoyos and colleagues found that upregulation of a gene called SMNDC1 in aggressive pancreatic cancer samples could stimulate the inclusion of cassette exons that may make proteins more oncogenic.

One example is exon 4 of MAPK3, an important gene for cell growth and proliferation. When cells had more SMNDC1, a higher percentage of MAPK3 transcripts had exon 4, which encodes phosphorylation sites that help activate the resulting protein, ERK. Therefore, without mutating MAPK3 or changing its expression, SMNDC1 could stimulate ERK activation via RNA splicing.
Escobar-Hoyos also briefly touched on the potential use of RNAs as pancreatic cancer therapeutics. Building on a lupus-derived antibody discovered in 1990 that can travel into cells and bind to DNA, Escobar-Hoyos and colleagues designed an RNA-binding antibody called TMAB and engineered it to bind to an immunogenic type of RNA called 3p-hpRNA, which mimics viral RNA. The researchers found that TMAB could bring 3p-hpRNA into pancreatic cancer cells and stimulate antitumor immune responses in mouse pancreatic tumors, leading to a tumor response that was superior to the standard-of-care chemotherapy gemcitabine.
Snippets of Success
This year, the keynote session also included six Lightning Talks, in which selected speakers discussed their cutting-edge advances in two-minute presentations. The talks highlighted crucial topics in pancreatic cancer research:
Equity in genetic testing. While germline genetic testing is recommended for all patients with pancreatic ductal adenocarcinoma (PDAC), a previous study by Xianghui Zou, MD, a resident physician at Northwell Health, and colleagues reported significant delays in genetic testing among patients of racial and ethnic minority groups and patients with lower incomes. In the present study, they re-evaluated these delays following an educational intervention about genetic testing. The median time to testing was 14 days in this study compared to 28 days in the previous study, and the association between lower income or racial/ethnic minority status and longer delays was no longer significant. “Overall, through a pretty cheap intervention—basically raising awareness amongst physicians and promoting same-day testing—we were able to decrease the median [delay] from 28 days to 14 days,” Zou said.
Imaging-based early detection. Positron emission tomography (PET) is a standard imaging technique to diagnose pancreatic cancer, but its utility in diagnosing early-stage PDAC could be improved, argued Yukihito Kuroda, PhD, a postdoctoral fellow at Columbia University presenting work done as a graduate student at the University of Tsukuba in Japan. Kuroda and colleagues previously found that fucosylated glycans, a type of cell surface tag, were abundant on early-stage PDAC cells, and they identified a recombinant lectin that can bind to these glycans. The researchers attached their lectin to the PET label N-succinimidyl-4-[18F]fluorobenzoate and showed that uptake into subcutaneous mouse PDAC cell xenografts was rapid, robust, and specific. “We believe a lectin-based PET probe warrants further clinical development to improve diagnostic accuracy and sensitivity,” Kuroda said.
How fats connect alcohol use to PDAC. Researchers have attempted to evaluate the effects of alcohol use on PDAC risk, but the results have been inconsistent. Sabine Naudin, PhD, MPH, and her colleagues at the National Institutes of Health and the International Agency for Research on Cancer, evaluated the relationship between self-reported alcohol use, serum concentration of 611 lipid species, and risk of PDAC development among 716 PDAC patients and matched controls. They found that increased alcohol use correlated with increases in 36 lipid species, but that 10 of these lipids were associated with decreased odds of PDAC. “All this work shows that there might be lipid pathways involved in this association,” Naudin said.
Monitoring cachexia progression. Cachexia, a progressive muscle wasting disease, occurs in around 80% of pancreatic cancer patients, said Deepti Mathur, PhD, a postdoctoral research fellow at Memorial Sloan Kettering Cancer Center. Because little is known about the molecular characteristics of cachexia development and progression, Mathur and colleagues performed a comprehensive metabolomic analysis in a mouse model of PDAC cachexia. In addition to identifying metabolites, especially lipids, that fluctuated in various tissues during cachexia progression, they also identified metabolic changes that occur prior to the onset of cachexia symptoms. “Combined with machine learning, we can extract metabolic markers which, based on early changes, could predict future cachexia development,” Mathur said.
Boosting chemotherapy response. Chemotherapy is a mainstay of pancreatic cancer treatment, but tumors often develop resistance. Previous studies showing robust upregulation of the gene IDH1 in chemotherapy-resistant PDAC prompted Mehrdad Zarei, PhD, a postdoctoral researcher at the Case Comprehensive Cancer Center of Case Western Reserve University, and colleagues to assess whether IDH1 was driving chemotherapy resistance, and if inhibiting IDH1 could boost chemotherapy efficacy. In cell and mouse models of PDAC, the IDH1 inhibitor ivosidenib (Tibsovo) synergized with chemotherapy to inhibit cell growth. “Based on these data, we have initiated a phase I clinical trial by combining ivosidenib and chemo drugs,” Zarei said.
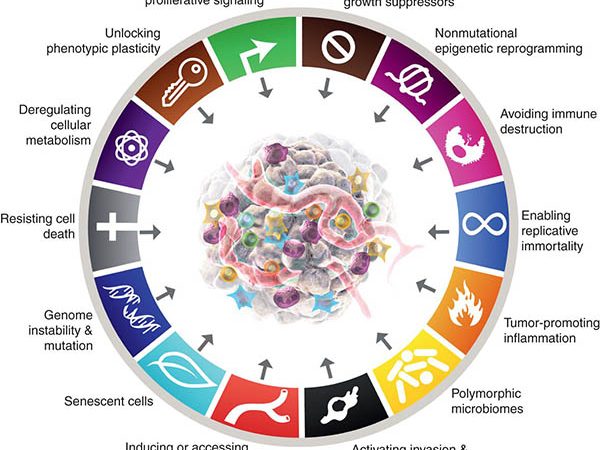
Predicting prognosis via epigenetics. When tumors develop, broad changes in DNA accessibility for transcription occur in both cancer cells and cells in the microenvironment, explained Kevin MacPherson, a graduate student in the Department of Molecular and Medical Genetics at Oregon Health and Science University. MacPherson and colleagues analyzed these changes by performing single-cell ATAC-seq (a technique that sequences accessible chromatin regions) on 42 PDAC samples and single-cell RNA-seq on 10 PDAC samples. They identified differences in chromatin accessibility between the basal and classical subtypes of PDAC and found evidence of robust T-cell remodeling by the tumor. “Epigenetics is the foundation upon which a cell’s identity is built,” MacPherson said. “Epigenetics has the means to explain both pancreatic cancer phenotypes and clinical outcomes.”