Symposium Explores Clinical Trial Design and Multidrug Resistance in Blood Cancers
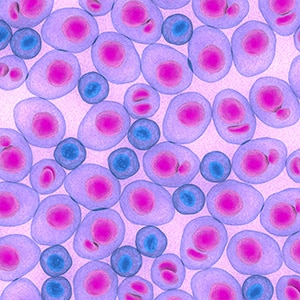
The treatment of blood cancers has taken giant leaps in recent years. The advent of immunotherapy and new targeted therapies for multiple myeloma, leukemia, and lymphoma have greatly expanded the arsenal of treatment options, helping many patients live longer.
Evolving treatment modalities and longer patient survival, however, necessitate rethinking of clinical trial strategies and interpretation of trial results. And while patients today have many more therapeutic options, treatment resistance unfortunately remains prevalent.
Recent progress in addressing these hurdles was discussed earlier this month at the Blood Cancer Discovery Symposium, organized by the editors of the eponymous American Association for Cancer Research (AACR) journal. In addition, Blood Cancer Discovery published two articles concurrent with meeting presentations: a research article uncovering a mechanism of multidrug resistance and a commentary on optimizing clinical trial design.
How does multidrug resistance develop in AML?
Approximately two-thirds of patients with acute myeloid leukemia (AML) experience disease relapse after chemotherapy or targeted therapy, according to Shruti Bhatt, PhD, an assistant professor at the National University of Singapore. In some cases, the patient may even develop resistance to drugs they have never received.
She and colleagues, including cosenior author Anthony Letai, MD, PhD, a professor at Harvard Medical School and Dana-Farber Cancer Institute, set out to answer a longstanding question in the field: How does exposure to a single agent lead to insensitivity to multiple agents?
“This is one of the most unsolved questions in oncology, as multidrug resistance is the root cause of death at relapse in most cancer patients,” said Bhatt, who completed her postdoctoral training in Letai’s lab. “Any discussion with oncologists or cancer biologists, or interrogation of the literature, rapidly reveals a paucity of models and reliable evidence, particularly in vivo, regarding the explanation for multidrug resistance in the relapse setting.”
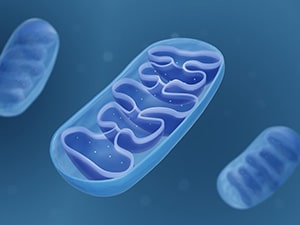
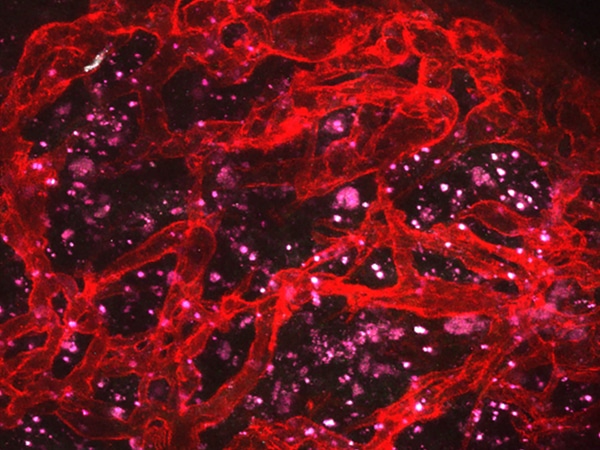
Together with Letai, who presented data on functional precision medicine in blood cancers at the Blood Cancer Discovery Symposium, Bhatt and colleagues developed mouse models of AML with acquired resistance to therapies targeting FLT3, BCL2, MCL1, BRD4, or apoptosis proteins. By studying gene expression in these mouse models and in parental mice, the researchers uncovered that resistance to any of the evaluated targeted therapies was associated with reduced mitochondrial priming despite each therapeutic’s distinct mechanism of action.
Mitochondrial priming refers to a cell’s threshold for apoptosis; cells with highly primed mitochondria stand ready to activate apoptosis and are more vulnerable to cytotoxic therapies. The findings from Bhatt, Letai, and colleagues suggest that when AML becomes resistant to one therapeutic, its threshold for cell death increases—meaning that it becomes less likely to succumb to any cytotoxic therapy, whether or not the cell has been previously exposed to it.
Further, the researchers demonstrated that a drug’s impact on mitochondrial priming, as measured by dynamic BH3 profiling (DBP), could predict its efficacy against multidrug resistant AML.
“These findings have huge implications for how we treat relapsed AML,” said Bhatt. “By using DBP-based measurements, we can now identify active therapy that is able to cause enhancement of mitochondrial apoptotic signaling in a patient-specific manner.”
This approach will be evaluated in an upcoming phase II clinical trial for patients with relapsed AML.
Bhatt predicts that reduced mitochondrial priming may underlie multidrug resistance in tumor types beyond AML as well, noting, “These findings for AML are only the tip of the iceberg for all human cancers.”
How can we improve clinical trials for smoldering multiple myeloma?
Currently, most cases of smoldering multiple myeloma (SMM) and other blood cancer precursor conditions are managed with a “watch and wait” approach, but recent advances are enabling early interventions to delay or even prevent progression to cancer.
Clinical trials that evaluate interventions for blood cancer precursor conditions, however, require unique considerations, according to a commentary by Irene Ghobrial, MD, and colleagues in Blood Cancer Discovery. The commentary was published simultaneously with a keynote address on this topic delivered by coauthor Nicole Gormley, MD, at the Symposium.
“The goal of new therapies in SMM or other hematologic precursor conditions is to … prevent or delay the development of symptomatic disease while minimizing toxicities and side effects,” Ghobrial, Gormley, and colleagues wrote.
To best meet this goal, they noted that changes are needed to multiple aspects of traditional clinical trial design—including risk stratification, dose optimization, selection of endpoints, assessments of safety and patient quality of life, and ensuring demographic diversity.
Identifying patients with the greatest risk of disease progression would allow researchers to tailor treatments to patients who are most likely to benefit, while avoiding overtreatment in patients whose SMM is unlikely to progress, the authors explained.
They also noted that traditional methods of dose optimization, which rely on the maximum tolerated dose, are not well suited to precursor conditions such as SMM. Since some patients may receive the treatment long term, the authors recommended that researchers instead strive to identify doses that minimize toxicity and adverse impacts on quality of life while still providing clinical benefit. The authors also suggested identifying a range of dosages to accommodate different patient populations and varying treatment durations.
Additionally, the authors discussed considerations for selecting trial endpoints. They explained that the long natural history of SMM makes it difficult to assess long-term endpoints, such as overall survival, and many earlier endpoints have not been validated in this setting. Another hurdle is that some patients may not want to delay treatment if their SMM shows signs of biochemical progression, but initiating treatment may complicate the assessment of progression to clinically defined multiple myeloma. The authors propose biochemical progression and sustained minimal residual disease as potential early endpoints for assessing the efficacy of therapeutics for SMM.
Finally, the authors emphasized the importance of diversity and inclusion in clinical trial populations, as the safety and efficacy of a drug may differ across demographic groups.
Together, the insightful findings published by Blood Cancer Discovery and discussed at its inaugural Symposium set the stage for treatment breakthroughs for various blood cancers—breakthroughs that could overcome treatment resistance and better evaluate new therapeutics for cancer precursor conditions.