Bloodlines Series: Risk, Regimens, and Research for Multiple Myeloma
Cancer Research Catalyst is proud to bring you Bloodlines, a new series focused on hematological malignancies (blood cancers). The Bloodlines series will cover everything from the basics of how blood cancers form to cutting-edge research improving patient outcomes. Our first installment discusses the evolving treatment landscape of multiple myeloma and how new research is giving patients more treatment options.
In April 2020, Darlene Pruess was a sommelier at a restaurant, an avid bike rider, and an artist who dabbled in carpentry and remodeling. A severe pain in her ribs sent her to the emergency department, where they discovered she was in acute kidney failure. A bit more probing led to a diagnosis of multiple myeloma, a blood cancer with many different treatment options.
Pruess immediately started a treatment regimen known as CyBorD, a combination of cyclophosphamide, bortezomib (Velcade), and dexamethasone. She then underwent a bone marrow transplant, followed by several different treatment combinations that led her in and out of remission. On a recent treatment regimen—consisting of cyclophosphamide, pomalidomide (Pomalyst), and dexamethasone—she has been able to enjoy many of the activities she loved before her diagnosis, like swimming and biking.
Despite the many rounds of therapy she’s tried, Pruess is grateful for the availability of different options that have kept her cancer at bay. “This is wonderful that, even though I continue to go back and forth in remission … they have individual recipes just for me that work,” she said.
Cycling through various regimens is a common experience for patients with multiple myeloma. Fortunately, new research has consistently managed to extend the list of options for patients facing this disease.
What is Multiple Myeloma?
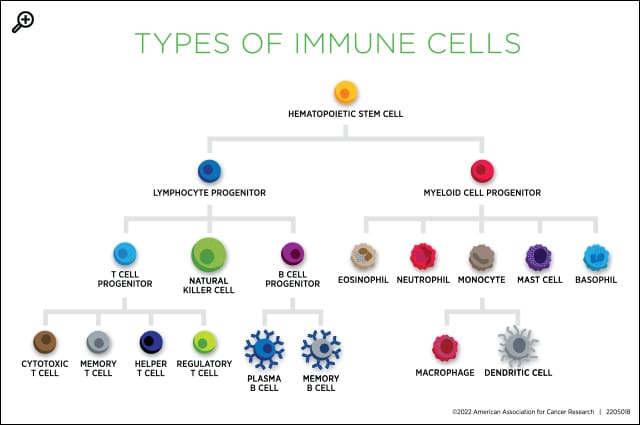
Blood cancers occur when the body makes immature or abnormal white blood cells. The abnormal cells don’t function properly and crowd out the healthy cells. Blood cancers are primarily classified based on the type of cell from which they arise. Multiple myeloma is a type of plasma cell neoplasm, meaning it forms from plasma cells, or B cells that produce antibodies.
The abnormal plasma cells of multiple myeloma build up in the bone marrow and can cause tumors in various bones. As a result, symptoms can vary widely, and some patients have no symptoms at all. Some symptoms associated with multiple myeloma may include bone pain (especially in the back or ribs), fragile bones, frequent infections and/or unexplained fever, bruising or bleeding easily, trouble breathing, weakness of the limbs, and fatigue.
The nonspecific nature of these symptoms can lead to delayed or incorrect diagnoses. Oya Gilbert visited the emergency department in 2015 for a suspected heart attack and was told it was just anxiety. For the next two years, he continued to experience episodes of debilitating pain, shortness of breath, and fatigue with no physical diagnosis. When doctors finally did a full workup in 2017, they found elevated levels of certain proteins in Gilbert’s blood and urine.
These protein tests are a common starting point for diagnosing multiple myeloma. Because the abnormal plasma cells produce antibodies, a buildup of antibody-associated proteins, including beta-2-microglobulin and free light chain, can indicate a problem. Abnormal plasma cells may also produce a factor called M protein that can be identified in blood and urine tests.
The next step in diagnosis is often a bone marrow biopsy. Gilbert’s biopsy confirmed a diagnosis of multiple myeloma in December 2017.
As Gilbert learned more about multiple myeloma, he also learned more about risk factors that may have played a role in his diagnosis. For instance, multiple myeloma is significantly more common in men than in women and in Black individuals than in white individuals. Other risk factors include exposure to radiation or chemicals and a family history of benign plasma cell neoplasms like monoclonal gammopathy of unknown significance (MGUS) and plasmacytoma.
Gilbert used his own experience to launch the Health, Hope, & Hip-Hop Foundation, a nonprofit that seeks to bring medical education and health equity to underresourced communities through the uniting force of hip-hop music. He expressed hope that improving health literacy in rural communities like the one where he was diagnosed may help benefit more patients in the future.
Treatment Options for Multiple Myeloma
According to the National Comprehensive Cancer Network (NCCN), first-line treatment for multiple myeloma is often a cocktail of different drugs that target the cancer cells in different ways. Combinations can vary, but most contain many or all of these components:
- a proteasome inhibitor, such as bortezomib or carfilzomib (Kyprolis);
- an immunomodulatory drug, such as lenalidomide (Revlimid), thalidomide (Thalomid), or pomalidomide;
- the steroid dexamethasone; and/or
- an antibody targeting the protein CD38, such as daratumumab (Darzalex) or isatuximab-irfc (Sarclisa).
In many cases, these regimens will be followed by a stem cell transplant, either using the patient’s own healthy stem cells or those from a donor. Before and/or after a transplant, patients may continue receiving part of their regimen for an extended time to reduce the risk of relapse. This was the case for Gilbert, who received bortezomib, lenalidomide, and dexamethasone before his stem cell transplant then continued taking lenalidomide afterwards.
If patients decline the transplant or are ineligible, or if their cancer returns after a transplant, they may receive additional combinations, as Pruess did. Sometimes, these can incorporate chemotherapies, such as cyclophosphamide, or other targeted therapies, such as venetoclax (Venclexta), a drug that stimulates cell death.
In recent years, new immunotherapies have entered the market to give patients with multiple myeloma additional treatment options. Two chimeric antigen receptor (CAR) T-cell therapies, ciltacabtagene autoleucel (Carvykti) and idecabtagene vicleucel (Abecma), have been approved by the U.S. Food and Drug Administration (FDA) to treat patients whose disease has recurred following treatment with various therapies. CAR T therapy is a type of cell therapy in which T cells are harvested from a patient, modified in a lab to enhance their cancer-fighting capabilities, expanded, and infused back into the patient.
Bispecific engager molecules have also proven effective against multiple myeloma. This innovative immunotherapy employs bispecific antibodies, molecules that can bind to two different targets on the same protein or on two different proteins. In the case of bispecific engagers for multiple myeloma, the engagers bind to the protein CD3 on T cells (a type of immune cell) and another protein on myeloma cells to bring the two into proximity. This helps the T cells attack the myeloma cells and kill the cancer.
Three bispecific engagers have been approved by the FDA for patients with multiple myeloma who have received at least four prior therapies:
- Teclistimab-cqyv (Tecvayli) targets the B-cell maturation antigen (BCMA) on multiple myeloma cells and was granted accelerated approval in 2022.
- Talquetamab-tgvs (Talvey) targets the protein GPRC5D on multiple myeloma cells and was approved in August 2023.
- Elranatamab-bcmm (Elrexfio) targets the protein CD38 on multiple myeloma cells and was also approved in August 2023.
Research Leads to New Treatment Options
Talquetamab-tgvs was a saving grace for Vicki W. Jones, who has battled multiple myeloma on and off since 2004. She began her treatment journey with chemotherapy, then a stem cell transplant, then she proceeded through many different treatment combinations over the next several years. Each new regimen worked for one to four years before she switched to something else, she recalled.
In 2023, Jones began receiving talquetamab-tgvs after hearing about the drug at a scientific conference a few years prior. So far, it has kept her cancer at bay, adding to the scientific progress that has kept her alive for over 20 years.
“I am incredibly lucky that progress in cancer research has been faster than the progression of my disease,” Jones said. “Without that, I wouldn’t be here, and I am so grateful.”
Multiple myeloma research continues to spur additional treatment options for patients. For instance, two new indications for CD38-targeting antibodies were approved by the FDA in 2024. Daratumumab and hyaluronidase-fihj (Darzalex Faspro) gained its eighth multiple myeloma approval in July for use in the induction and consolidation phases of therapy in combination with bortezomib, lenalidomide, and dexamethasone. A new indication for isatuximab-irfc followed in September, also with bortezomib, lenalidomide, and dexamethasone, for the first-line treatment of patients who aren’t eligible for a stem cell transplant.
What’s next on the horizon? Blood Cancer Discovery, a journal of the American Association for Cancer Research (AACR), has a collection of exciting multiple myeloma advances being published in the journal. Keep an eye out there for new basic, translational, and clinical research that may help improve outcomes for patients.



