AACR Virtual Annual Meeting I: A Global Perspective of COVID-19 in Patients with Cancer
At the time of this writing, more than 3.3 million individuals have been diagnosed with COVID-19, and more than 222,000 have died from the disease worldwide. The United States recently exceeded 1 million confirmed cases, resulting in more than 62,000 deaths.
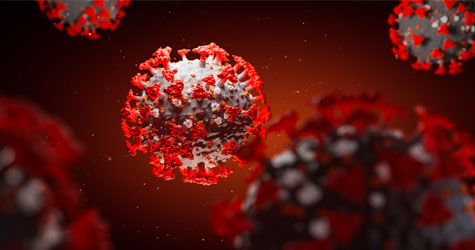
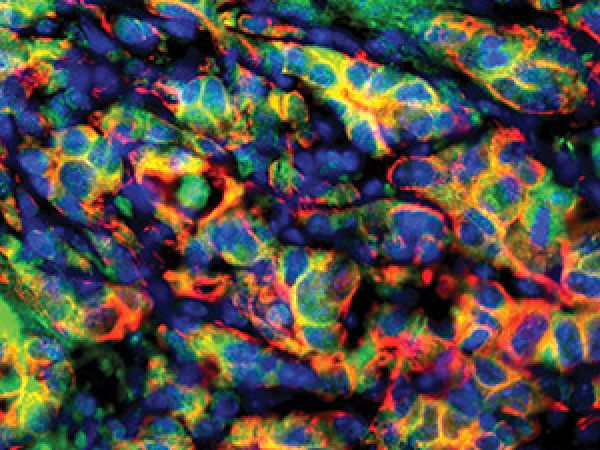
While COVID-19 can affect anyone, some populations are more sensitive to severe infection. Those aged 65 or older, for example, have higher rates of hospitalization and death. The experience of patients with cancer and COVID-19 is an area of active investigation, and whether this patient population has an increase in adverse outcomes following infection with SARS-CoV-2, the coronavirus which causes COVID-19, is an important question that will inform patient care.
Studies focused on COVID-19 and cancer are beginning to emerge. Articles in JAMA, Lancet Oncology, and Annals of Oncology, for example, have assessed the percentage of patients with cancer among those hospitalized with COVID-19 and compared the outcomes of patients with cancer with outcomes of the general population with COVID-19, in New York and China. These studies report varying percentages of patients with cancer, and varying associations between cancer and mortality in COVID-19 patients, and further research will be necessary to fully understand the global impact of COVID-19 on the cancer community.
The second day of the AACR Virtual Annual Meeting I began with a plenary session focusing on COVID-19 and cancer. Talks in this session highlighted global experiences combating COVID-19 among patients with cancer, the creation of an international registry of patients with thoracic cancers, and a look at disparities in patients with COVID-19. Data from a couple of studies indicate an increased risk of death from COVID-19 in patients with cancer; further studies are required, however, to ascertain this fact.
Large cohort studies from China and New York showed increased odds of death
A pair of studies recently published in the AACR journal Cancer Discovery evaluated how patients with cancer fare after contracting COVID-19 compared with those without cancer. One study evaluated outcomes of patients treated in Hubei Province, China, while the second study looked at outcomes of patients treated in New York City. Both studies found that patients with cancer had significantly increased odds of death.
The New York study evaluated 218 patients with cancer and COVID-19 treated in the Montefiore Health System from March 18 to April 8, 2020. Of these patients, nearly 30 percent died from COVID-19. Mortality rates among patients with cancer revealed that those with lung cancer, gastrointestinal cancers, gynecologic malignancies, and hematologic malignancies had the highest rates of death. Overall, the researchers identified several factors that significantly increased patients’ odds of death, including older age, multiple comorbidities, admission to the intensive care unit, and elevated inflammatory markers.
To determine if patients with cancer had higher mortality rates from COVID-19 compared with the general population, the researchers evaluated an age- and sex-matched cohort of more than 1,000 patients with COVID-19 without cancer treated at the same hospital system during the same time period. They found that patients with cancer had more than twice the odds of death. Further, when the researchers compared mortality outcomes from the patients with cancer in this study with COVID-19 mortality data spanning all New York City cases as of April 12, they found that patients with cancer had over six times the odds of death. The estimated mortality rate from COVID-19 in New York City as of April 12 was 6 percent.
The Chinese study, which was presented by Hongbing Cai, MD, from Zhongnan Hospital of Wuhan University during the COVID-19 and Cancer plenary session at the AACR Virtual Annual Meeting I, examined data from 641 patients with COVID-19 collected from 14 hospitals. Of these hospitalized patients, 105 had cancer. Those without cancer were matched by the same hospital, hospitalization time, and age to generate a control group. Patients were enrolled in this study between January 1 and February 24, 2020.
Compared with patients with COVID-19 without cancer, those with cancer and COVID-19 had over twice the odds of death. Further, patients with cancer had roughly three times the odds of intensive care unit (ICU) admissions, had nearly three times the odds of developing at least one severe or critical symptom, and had significantly higher odds of invasive mechanical ventilation. When the researchers stratified patients by cancer stage, they found that those with metastatic disease had an increased rate of severe events. The associations were stark: Patients with stage 4 cancer had more than five times the odds of death. Patients with localized cancer, on the other hand, had similar outcomes to those without cancer.
The researchers evaluated associations between cancer treatment type (received within 40 days before the onset of COVID-19 symptoms) and rates of severe events. They found that patients who received immunotherapy had the highest odds of death, and patients who received immunotherapy or surgery had the highest odds of developing a severe or critical symptom. At the close of her presentation, Cai noted that individualized treatment plans need to be developed based on both cancer type and cancer stage.
Another outlook from China
Li Zhang, MD, from Tongji Hospital in Wuhan, China, reviewed findings from her study, recently published in Annals of Oncology, that detailed the clinical characteristics of patients with both cancer and COVID-19 from three hospitals in Wuhan.
Of the 1,276 patients with COVID-19 admitted to the three designated hospitals, 28 had cancer, representing 2.2 percent of the total patients. Zhang noted that the estimated incidence of cancer in the Chinese population is 0.29 percent, suggesting that patients with cancer may be more susceptible to COVID-19 infection.
Of the 28 patients with cancer who contracted COVID-19, 25 percent had lung cancer; the second most common type of cancer was esophageal cancer. Almost 30 percent of patients were suspected to have hospital-associated transmission of COVID-19, and nearly 60 percent of patients had severe events, which were defined as a condition requiring admission to the ICU, the use of mechanical ventilation, or death.
Almost 30 percent of patients with cancer and COVID-19 died. Of these patients, the predominant cause of death was acute respiratory distress syndrome (ARDS).
The researchers found that those treated with an anticancer treatment within 14 days of their COVID-19 diagnosis, or those with a patchy lung consolidation on their computed tomography (CT) scan upon admission, had the highest risk of severe events.
A focus on France
Fabrice Barlesi, MD, PhD, from the Gustave Roussy Cancer Campus in Villejuif, France, outlined the outcomes of 137 patients with cancer infected with SARS-CoV-2 who were treated at Gustave Roussy from March 14 to April 15, 2020. The data cutoff was April 20, and the median follow-up time was 13 days.

Most patients had solid tumors (119 patients), with breast cancer being the most common cancer. Approximately 60 percent of patients had advanced disease, while around 40 percent were in remission or were being treated for localized disease. More than 20 percent of patients were asymptomatic for COVID-19.
Roughly 25 percent of patients exhibited clinical worsening, defined as the need for oxygen supplementation of 6 liters/minute or more, or death of any cause. Eleven percent of patients were admitted to the ICU, and nearly 15 percent of patients died. All fatalities were related to COVID-19. A significant predictor of clinical worsening was having an Eastern Cooperative Oncology Group (ECOG) status greater than 1. Other predictors of clinical worsening included having a hematological cancer or having received chemotherapy treatment within the last three months. Among these patients treated with chemotherapy, those with metastatic disease had an increased risk of death, while those with localized disease did not, as compared with patients that did not receive a recent chemotherapy treatment.
Barlesi noted that the mortality rate of patients with cancer and COVID-19 at Gustave Roussy (14.6 percent) was comparable to the estimated mortality rates from COVID-19 in both the Paris area (18.3 percent) and in France overall (17.9 percent) at the time of the study.
Perspectives from Spain

Carlos Gomez-Martin, MD, PhD, from University Hospital 12 de Octubre in Madrid, Spain, talked about his experiences treating patients with COVID-19 and cancer. He outlined information pertaining to the first 63 patients with cancer and COVID-19 admitted at his institution. The most common types of malignances were lung and gastrointestinal cancers. Over 80 percent of patients had metastatic disease, and 40 percent of patients had lung involvement, either in the form of primary or metastatic cancer.
Approximately 25 percent of patients died from COVID-19. More than half of patients developed respiratory failure, and nearly 40 percent developed ARDS.
Gomez-Martin noted that patients with cancer with lung involvement, an ECOG status of 2 or higher, severe neutropenia, or those with bilateral lung infiltrates during their baseline CT scan had significantly increased mortality.
Experience with anti-IL-6 treatment in Italy
Paolo A. Ascierto, MD, from the Istituto Nazionale Tumori IRCCS Fondazione Pascale in Naples, Italy, talked about the use of the anti-IL-6 drug tocilizumab (Actemra) for the treatment of patients with severe COVID-19. Tocilizumab is approved to treat patients who have cytokine release syndrome, and research suggests that this drug may be an effective treatment for some patients with severe COVID-19. Ascierto and colleagues began using tocilizumab for patients with respiratory distress in March, and he outlined two case studies where this treatment resulted in improved recovery.

Based on these results, Ascierto and colleagues initiated a phase II clinical trial evaluating tocilizumab in patients with COVID-19 pneumonia.
Ascierto also talked about the use of the anti-IL-6 drug sarilumab (Kevzara) in 15 patients with severe COVID-19. Ten of these patients responded, and Ascierto highlighted a couple of cases in which patients responded within 72 hours. The use of sarilumab is also being evaluated in a phase II clinical trial for patients with COVID-19.
TERAVOLT: a global collaboration for patients with thoracic cancers who contract COVID-19

Once it became clear that the COVID-19 pandemic would not last for days, but rather for months or longer, Marina Chiara Garassino, MD, from Istituto Nazionale dei Tumori in Milan, and colleagues decided to create a registry to address the impact of COVID-19 in patients with thoracic cancers. The idea for this registry – coined TERAVOLT – was born on March 15, during the peak of the outbreak in Italy. As of April 20, there were over 260 patients spanning 21 countries included in the registry. Garassino presented data from the first 200 patients enrolled in this global consortium.
So far, in this registry, nearly 74 percent of patients have advanced disease. The most common type of cancer is non-small cell lung cancer (NSCLC), comprising over 75 percent of patients. More than 80 percent of patients have pre-existing comorbidities, the most common being hypertension (over 45 percent), followed by chronic obstructive pulmonary disease (COPD; over 25 percent). No comorbidities were significantly associated with a higher risk of death.
The most reported complication in this patient population was pneumonia/pneumonitis, affecting almost 80 percent of evaluable patients. Further, almost 27 percent of patients had ARDS. Over 75 percent of patients were hospitalized, and almost 35 percent of patients died, either at the hospital, in the ICU, or at home.
“Our data suggest an unexpectedly high mortality among thoracic cancer patients,” Garassino noted. The cause of death in the large majority of patients is attributed to COVID-19 and not cancer, she said. She highlighted that many patients were not offered ICU admissions, possibly due to shortages or institutional rules.
“Things are moving quickly,” Garassino said, noting that this collaboration is registering roughly 70 patients per week from across the globe. “With a strong united thoracic community, we were able to activate a global registry and provide preliminary data in only one month, in absence of dedicated funding.”
Flattening the curve – but widening the disparities – during the COVID-19 pandemic
“The issues of racial and ethnic disparities are not novel,” began Louis P. Voigt, MD, from Memorial Sloan Kettering Cancer Center in New York. This issue has carried over to the COVID-19 pandemic, as racial and ethnic minorities carry a disproportionate burden of hospitalization and death.

A look at racial demographic data reveals stark disparities in COVID-19 deaths in New York City. Black/African American New Yorkers are dying at twice the rate of their white peers, said Voigt. Additionally, Hispanic/Latino New Yorkers have disproportionally high rates of death compared with white or Asian New Yorkers. Similar trends are seen in infection and hospitalization rates.
“Pandemics create perfect conditions for suboptimal care, or deviation from standard care, with major impact on the most vulnerable patients among us,” Voigt said.
“The most vulnerable among us can fall through the safety net if we do not pay attention,” he stressed. “We need to create a more robust safety net to shield them from the effects of cancer and COVID-19, because the disparities and other social determinants of health put them in a much higher category of vulnerability.”
What’s next?

“The full effect of the COVID-19 pandemic on patients with cancer and cancer researchers has yet to become clear,” said AACR President-Elect Antoni Ribas, MD, PhD, FAACR, and Program Committee Chair for this year’s annual meeting, during the Opening Session. To aid in the global COVID-19 response, the AACR recently announced a COVID-19 and Cancer Task Force. “The newly formed task force will provide leadership and insight to the AACR on issues surrounding the COVID-19 pandemic, focusing on high-impact initiatives,” said Ribas, who chaired the session on COVID-19 and cancer.
As the field is evolving rapidly, the AACR will include sessions on COVID-19 and cancer in Virtual Annual Meeting II, held June 22-24. The AACR is also holding a dedicated meeting focused on COVID-19 and cancer in July, and a call for abstracts on this topic will be circulated soon. Stay tuned for more information.