Bladder Cancer Awareness Month: Recent Developments in Risk Reduction and Treatment
Bladder cancer is a common malignancy originating in the bladder, a hollow organ located in the abdomen that stores urine. It is the sixth most prevalent cancer in the United States and has a high rate of recurrence. Over 90 percent of bladder cancers are urothelial carcinomas, which originate in the innermost tissue layer of the bladder lining.
Bladder cancer is most frequently diagnosed in men and in individuals over 65 years of age. Several additional factors may increase an individual’s risk, including smoking, having a family history of the disease, certain genetic mutations, and exposure to certain chemicals.
While patients diagnosed with early-stage disease have a relative five-year survival rate of 95.8 percent, patients diagnosed after the disease has spread to other organs have a five-year survival rate of only 5.5 percent. Over half of bladder cancers are diagnosed when the cancer cells are still localized to the tissue layer in which they originated; this stage of cancer is referred to as carcinoma in situ.
In honor of Bladder Cancer Awareness Month, here are some of the latest advances in preventing and treating this disease.
Reducing the risk of bladder cancer
While many of the risk factors for bladder cancer cannot be altered, certain lifestyle changes may help reduce the risk of this disease. A study published last year in Cancer Prevention Research, a journal of the American Association for Cancer Research (AACR), found that quitting smoking reduced bladder cancer risk in postmenopausal women. The risk was reduced by 25 percent for the first 10 years after quitting compared with women who had not quit smoking. However, the risk of bladder cancer for former smokers remained higher than that of never-smokers. A recent study showed that several substances linked to bladder cancer were detected in the urine of e-cigarette users.
In another study published in Cancer Prevention Research, researchers used rat models of bladder cancer to examine whether non-steroidal anti-inflammatory drugs (NSAIDs) and/or inhibitors of the epidermal growth factor receptor (EGFR) could reduce the risk of developing bladder cancer. Both NSAIDs and EGFR inhibitors have been suggested to prevent bladder cancer, but daily dosing of these drugs is associated with various toxicities. In this study, the researchers investigated an alternate dosing schedule in which the drugs were administered once a week or on a three weeks on/three weeks off schedule. They found that rats that received these drugs on an alternate dosing schedule had fewer tumors and reduced tumor volume compared with untreated rats, raising the possibility that these drugs could eventually be used to reduce the risk of bladder cancer in high-risk individuals.
Treating patients with bladder cancer
For those who develop bladder cancer, treatment may include surgery, radiation therapy, chemotherapy, and/or immunotherapy. While there are multiple therapeutic options available to treat bladder cancer, there remain several challenges, including resistance or lack of response to certain treatments. Ongoing research continues to provide insight into potential strategies for addressing these challenges.
Treating patients whose bladder cancers are resistant to BCG
Since the 1970s, the bacterium Bacillus Calmette-Guérin (BCG) has been used as an immunotherapy to treat non-muscle invasive bladder cancer (NMIBC), which is cancer that is localized to the lining of the bladder. BCG is a weakened form of the bacterium that causes tuberculosis in cows and is used as a vaccine for tuberculosis in humans. When administered into a patient’s bladder, BCG stimulates the immune system, leading to local antitumor immune activity.
While BCG is effective for over 50 percent of patients with NMIBC, many patients have tumors that are resistant to this therapy and thus have limited treatment options. A recent study examined the clinical efficacy of an investigational gene therapy for patients with BCG nonresponsive NMIBC. The therapy, nadofaragene firadenovec, uses a viral vector to deliver the immune-stimulating IFNα2b gene directly into the bladder. Once in the bladder, the encoded IFNα2b protein activates a local immune response that can target bladder cancer cells.
In this phase III trial, 157 patients with BCG nonresponsive NMIBC were treated with nadofaragene firadenovec. Within three months of treatment, 53.4 percent of 103 patients with carcinoma in situ experienced complete responses, and 45.5 percent of these patients were free of high-grade recurrence after 12 months. Furthermore, most of the observed treatment-emergent adverse events were transient. These results demonstrate that nadofaragene firadenovec may be a promising treatment option for BCG nonresponsive NMIBC.
Another recent study, published in the AACR journal Clinical Cancer Research, examined the mechanisms underlying resistance to BCG. The study found that bladder cancers that did not respond to BCG were more likely to express the immune checkpoint protein PD-L1, suggesting that immune checkpoint activation may contribute to resistance to BCG. While additional research is needed, these findings raise the possibility that combining BCG with an immune checkpoint inhibitor could benefit some patients with BCG nonresponsive NMIBC.
Treating patients with immune checkpoint inhibitors
In recent years, several inhibitors of the PD-1/PD-L1 immune checkpoint pathway have been approved by the U.S. Food and Drug Administration (FDA) for the treatment of bladder cancer. The immune checkpoint inhibitors approved for bladder cancer are pembrolizumab (Keytruda), atezolizumab (Tecentriq), nivolumab (Opdivo), durvalumab (Imfinzi), and avelumab (Bavencio).
Results from a study published in the AACR journal Clinical Cancer Research suggest that inhibition of another immune checkpoint pathway – the CTLA-4 pathway – may be an effective treatment for bladder cancer as well. The publication reported results from a phase II clinical trial that evaluated the anti-CTLA-4 antibody tremelimumab in 32 patients with metastatic bladder cancer. The overall response rate was 18.8 percent, with two complete responses and four partial responses. The median overall survival was 10.3 months. The results of this study suggest that inhibition of CTLA-4 may provide clinical benefit for patients with metastatic bladder cancer.
Recent drug approval for bladder cancer
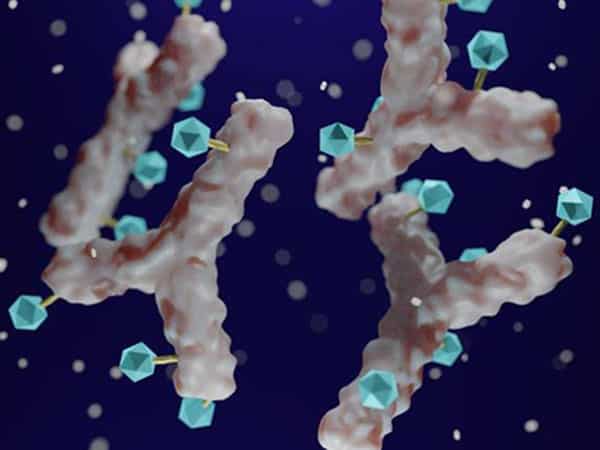
Preclinical studies and clinical trials like the ones described above are essential to the development and approval of new drugs and therapies. Following promising clinical trial data, the antibody-drug conjugate enfortumab vedotin-ejfv was approved by the U.S. Food and Drug Administration (FDA) in December 2019 for patients with locally advanced or metastatic urothelial cancer that has progressed after treatment with an immune checkpoint inhibitor and a platinum-based chemotherapy regimen. This drug targets a cellular protein called nectin-4, which is expressed at high levels on the surface of bladder cancer cells, and delivers a microtubule-disrupting agent that is toxic to the cancer cell, according to results from a 2016 study published in the AACR journal Cancer Research. You can read more about this drug approval in a blog post from December.
Surviving bladder cancer
Clinical trials and advances in treatment can improve survival for patients with bladder cancer. Dave Maddison and Gary Price both survived metastatic bladder cancer after participating in clinical trials for investigational immunotherapy and targeted therapy, respectively. You can read Dave’s story here, and Gary’s story here.



thank you for sharing helpful information about bladder cancer . It’s really very useful for the reader.