AACR Virtual Annual Meeting I: Innovative Immunotherapeutic Strategies
Clinical trials were a major focus of the AACR Virtual Annual Meeting I, spanning nine plenary sessions over the two-day conference.
“We determined that the program for the first Virtual Annual Meeting should focus largely on clinical trials and on the first disclosures of innovative small molecules and biologics that have recently entered phase I clinical trials, because we believe it is imperative that these data are disseminated rapidly to ensure that they yield maximum patient benefit,” said AACR President-Elect Antoni Ribas, MD, PhD, FAACR, and Annual Meeting Program Committee Chair during the Opening Session.
The first immunotherapy clinical trial plenary session, held during the opening day of the meeting, drew over 21,000 live views. Talks in this session focused on early-stage clinical trials that evaluated immunotherapeutic strategies such as a DNA vaccine, an mRNA-based treatment, and the inhibition of the immune checkpoint protein PVRIG. Findings from these clinical trials are summarized below.
Inhibition of the immune checkpoint protein PVRIG
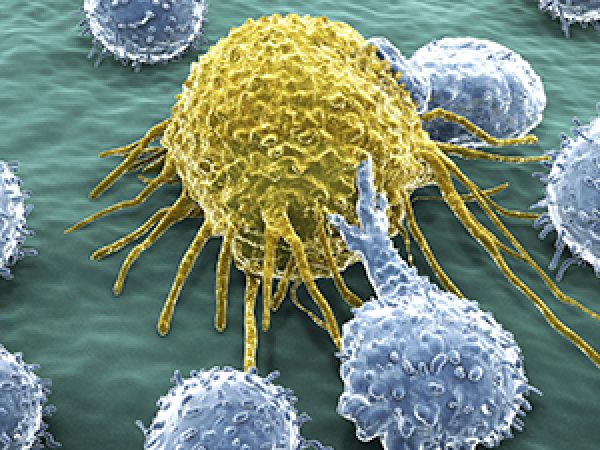
The inhibition of immune checkpoints—regulatory proteins that act as “brakes” on immune cells—is a therapeutic strategy that has fueled the immunotherapy revolution, resulting in unprecedented and durable responses in select patients. As such, several immune checkpoint inhibitors, such as those that inhibit PD-1, PD-L1, and CTLA-4, have become standard-of-care cancer treatments. Still, many patients do not respond to immune checkpoint inhibition, and many develop resistance to these therapies. Finding ways to enhance the efficacy of these immune checkpoint inhibitors—or identifying new checkpoint pathways to target—is a key area in immunotherapy research.
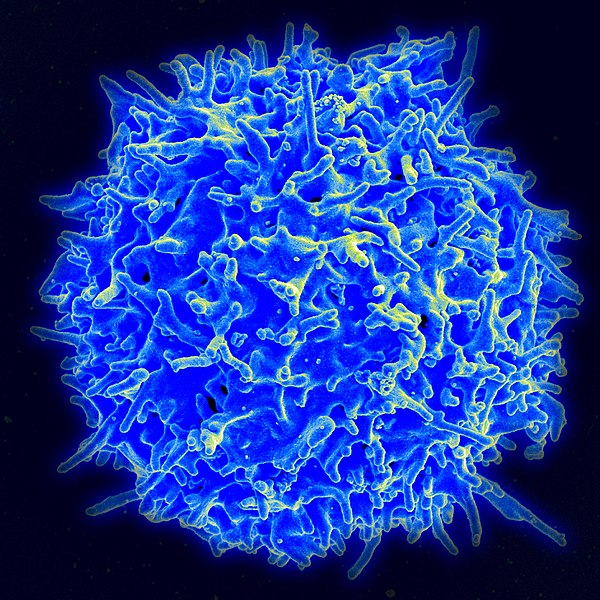
The poliovirus receptor-related immunoglobulin (PVRIG) is a cell surface receptor that is found on T cells. Similar to PD-1, when PVRIG interacts with its ligand PVRL2, which is overexpressed on the surface of many types of cancer cells, the T cell is “turned off” and the cancer cell is able to evade the immune response. Another receptor that is found on T cells, TIGIT, plays a similar role: Interaction with its ligand PVR leads to negative regulation of the T cell. Both PVRL2 and PVR can also bind to DNAM, a third receptor expressed on T cells, which leads to positive regulation and enhances T-cell function. Whether modulation of the DNAM axis can be exploited as a potential anticancer strategy is currently under investigation.
Ryan Sullivan, MD, from Massachusetts General Hospital, opened up the first immunotherapy clinical trial plenary session by discussing results from a phase I trial that evaluated the anti-PVRIG monoclonal antibody COM701 alone or in combination with the anti-PD-1 monoclonal antibody nivolumab (Opdivo) in patients with advanced solid tumors. Preliminary antitumor activity of COM701 (as a monotherapy) was previously reported at the 2019 Society for Immunotherapy of Cancer meeting. In this follow-up presentation, Sullivan provided an update of the monotherapy cohort and described the preliminary safety and antitumor activity of the COM701-nivolumab combination.

Sullivan explained the rationale for the dual inhibition of two checkpoint pathways: Because the PD-1/PD-L1 pathway negatively regulates DNAM signaling, “co-inhibition of PD-1, PVRIG, and/or TIGIT is logical and promising,” he said. He highlighted preclinical data that demonstrated the combined effect of PVRIG and PD-L1 inhibition in mouse models.
In this report, 16 patients treated with COM701 monotherapy and 12 patients treated with COM701 plus nivolumab were evaluable for dose-limiting toxicities (DLT) and treatment response. No DLTs were observed in either arm. Data showed no increase in toxicity when COM701 was combined with nivolumab.
In each cohort, one partial response was observed. The responder in the monotherapy arm had primary peritoneal cancer, while the responder in the combination arm had colorectal cancer. Both of these patients had microsatellite stable disease that had progressed following multiple prior lines of chemotherapy, and neither of these patients were predicted to respond to immune checkpoint inhibition, Sullivan noted.
Ten patients in the monotherapy cohort and eight patients in the combination cohort had stable disease. Two patients in the monotherapy cohort (one patient with adenoid cystic carcinoma and one patient with colorectal cancer) and four patients in the combination cohort (patients with anal squamous cell carcinoma, colorectal cancer, endometrial cancer, and non-small cell lung cancer) have had stable disease for at least six months, Sullivan said.
Overall, the disease control rate, defined as the combination of patients exhibiting a complete response, partial response, or stable disease, was 69 percent in the monotherapy arm, and 75 percent in the combination arm.
Sullivan noted that a phase I/II trial, which is evaluating the triplet combination of COM701, nivolumab, and the anti-TIGIT monoclonal antibody BMS-986207, is currently in development.
Stimulating OX40 via intratumoral injection
Modulation of the co-stimulatory immune checkpoint protein OX40 is another avenue of therapeutic investigation in the immunotherapy field. In the presence of a tumor neoantigen, the interaction between OX40 and its ligand, OX40L, can enhance the expansion of T cells, increase T-cell memory, and inhibit T regulatory cells, explained Antonio Jimeno, MD, from the University of Colorado Cancer Center, during his talk at this plenary session.
Jimeno presented data from a clinical trial that evaluated mRNA-2416, a therapeutic strategy that uses an mRNA encoding human OX40L encapsulated in a lipid nanoparticle. These nanoparticles are administered via intratumoral injection where they direct the cellular expression of endogenous-like OX40L protein, Jimeno said. This method has shown preclinical efficacy in mice, both alone and in combination with PD-L1 blockade.

In his talk, Jimeno described data from 39 patients with heavily pretreated relapsed/refractory solid tumors or lymphoma who received mRNA-246 monotherapy. More than half of these patients had previously been treated with an immune checkpoint inhibitor. No DLTs were observed following mRNA-246 monotherapy, and most treatment-related adverse events were grade 1 or 2.
Of the 39 patients, no partial or complete responses were observed. However, 14 patients had stable disease. Of the six patients with ovarian cancer, four had stable disease. Further, six patients had stable disease for at least 14 weeks, Jimeno noted.
When the researchers evaluated patients’ lesions, they found that two patients had tumor shrinkage in both injected and uninjected lesions, two patients had tumor shrinkage in injected lesions only, and three patients had tumor shrinkage in uninjected lesions only. “This shows that [mRNA-]2416 is able to induce both a direct immune response, as well as a systemic, distant effect,” Jimeno said.
The researchers also analyzed biopsies taken before and after treatment from a subset of patients. They found that most of the injected lesions had increased OX40L protein expression, increased levels of PD-L1 mRNA, and an increase in a T cell-inflamed gene expression profile score, which is predictive of anti-PD-1/PD-L1 response.
Jimeno noted that the evaluation of mRNA-2416 in combination with the anti-PD-L1 inhibitor durvalumab (Imfinzi) is currently ongoing, with a focus on patients with advanced ovarian carcinoma.
Pembrolizumab plus a therapeutic DNA vaccine
The use of therapeutic vaccines represents another treatment strategy in the immunotherapy field. By using tumor-specific antigens, therapeutic vaccines are designed to stimulate the immune system to target and attack a malignant tumor. A variety of therapeutic vaccines—either used as a monotherapy, or paired with an immune checkpoint inhibitor—are currently under evaluation.
Jung Won Woo, PhD, from Genexine Inc., presented an interim analysis from a phase II clinical trial that is evaluating the vaccine GX-188E in combination with the PD-1 inhibitor pembrolizumab (Keytruda) in patients with advanced, inoperable, or metastatic cervical cancer that is positive for human papillomavirus (HPV) types 16 and/or 18. These are high-risk HPV types that are responsible for about 70 percent of cervical cancers.
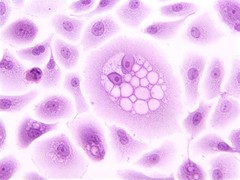
GX-188E is a DNA vaccine designed to preferentially induce antigen-specific CD8 T-cell responses, explained Woo. The vaccine, which is delivered intramuscularly by electroporation, facilitates the selective delivery of HPV antigens to dendritic cells. Previous phase I and phase II trials have demonstrated the safety and early therapeutic efficacy of GX-188E monotherapy in patients with high-grade cervical intraepithelial neoplasia (CIN) caused by HPV 16/18.
At the time of Woo’s presentation, 26 patients were evaluable for response. The objective response rate was 42.3 percent, which included four complete responses and seven partial responses. Four patients had stable disease, and 11 patients had progressive disease. The objective response rate among patients with PD-L1-positive tumors was 50 percent.
All patients who had a complete response had HPV-16 positive, PD-L1-positive squamous cell carcinoma. However, clinical responses were also observed in patients that had PD-L1-negative tumors, in patients with HPV-18-positive disease, and in patients that had adenocarcinoma.
Woo compared the efficacy and safety results with a report which described a cohort of 98 patients with advanced cervical cancer treated with pembrolizumab monotherapy in the clinical trial Keynote-158. When patients were treated with pembrolizumab alone, the objective response rate was 12.2 percent, which included three complete responses and nine partial responses. Among patients with PD-L1-positive tumors, the objective response rate was 14.6 percent. This trial led to the approval of pembrolizumab for patients with advanced cervical cancer following disease progression during or after chemotherapy.
The safety profile of the combination of GX-188E and pembrolizumab was comparable to the results reported in patients who received pembrolizumab monotherapy.
Woo concluded her presentation by noting that the combination of GX-188E and pembrolizumab is a safe and efficacious treatment for patients with advanced cervical cancer driven by HPV 16/18.
Stay tuned
The latest developments in immunotherapy treatments will continue to be featured in the AACR Virtual Meeting II, to be held June 22-24. Access to this meeting will be made freely available.