Advancing Molecular Epidemiology
An early collaboration between AACR Fellows Joseph F. Fraumeni, MD, and Frederick P. Li, MD, defined one of the first cancer predisposition syndromes linked to the most commonly mutated gene across all cancer types.
In 1962, the Beatles released their first single, Love Me Do; astronaut John Glenn became the first American to circle the earth; John F. Kennedy was the U.S president; and the origins of cancer and its many facets were largely unexplored.
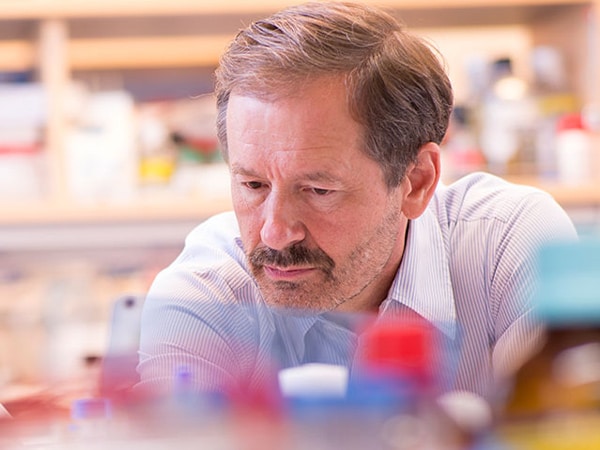
This is the intellectual setting in which Joseph F. Fraumeni Jr., MD, FAACR, began a trek that would make medical history by defining one of the first cancer predisposition syndromes that is linked to the most commonly mutated gene across all cancer types.
Li-Fraumeni syndrome—named for Dr. Fraumeni and his colleague Frederick P. Li, MD, FAACR—is a rare syndrome linked to the familial development of early-onset breast cancer, sarcomas, brain tumors and other malignancies. Prior to the time of their discoveries, little was known about heredity and cancer.

“In the 1960s, and even in the 1970s, cancer was a black box,” Dr. Fraumeni recalled. “We really didn’t have much information about what caused cancer.”
Scientists were beginning to explore the role of environmental factors such as smoking, based on some early studies and the Surgeon General’s 1964 report on smoking and health.
But little was known about the role of genetics in cancer. Although evidence was mounting for the existence of families in which several members experienced one of these cancers, often before the age of 50, a hereditary basis for cancer was a tough sell. When it did come up as a factor, the prevailing notion was that it was tissue- or site-specific. Drs. Fraumeni and Li would soon strike up a collaboration that would change that thinking.
A match made in Bethesda
Dr. Fraumeni had already been at the National Cancer Institute (NCI) of the National Institutes of Health (NIH) for five years when he first met Dr. Li.
“I had completed my residency in medicine with an interest in cancer, so I was very clinically oriented. Fred, on the other hand, came five years later. He had a passion for public health and global health and for working in underserved populations that were at high risk of various diseases,” Dr. Fraumeni said.
At the time, Dr. Fraumeni had started to explore the epidemiologic patterns of childhood and familial cancer with another NCI colleague, Dr. Robert W. Miller. While making rounds at the NIH Clinical Center, Dr. Fraumeni began looking into a series of cancer-prone families in the medical records. Soon after, another interesting case of familial occurrence came to the attention of Dr. Li.
It did not take long for Drs. Fraumeni and Li to become a de facto detective team.
One tumor they studied was rhabdomyosarcoma, a soft tissue sarcoma that frequently affects skeletal muscles and is most commonly diagnosed in children and adolescents. They noticed there was a lot of aggregation of cancer in the families that displayed a history of this type of tumor.
“It was one that tended to occur in siblings. Whenever that occurred, a parent would also come down with cancer at a very young age. It could be acute leukemia. It could be breast cancer,” said Dr. Fraumeni.
“Fred and I thought that there was something going on that was very important. We didn’t know what.”
The two doctors began to look for additional clues. Was it something in the environment? Was it a virus? Or perhaps, was it just a fluke?
Finally, they got a break by examining the charts of two cousins who lived apart from one another, but who both were diagnosed with rhabdomyosarcoma.
“So, we raised the possibility of a genetic factor. Because in one case acute leukemia occurred in the father. The other one was breast cancer in the mother. And both cases occurred in their early twenties,” said Dr. Fraumeni.
When they examined the family tree more deeply, they found many other types of cancer in the line of descent.
Acting on their hunch that there was an underlying genetic cause, the two doctors sifted through medical charts of other families in which soft tissue sarcomas were common. The search revealed there were many different cancers in those other families as well.
“We felt that this was something important,” Dr. Fraumeni said. “If we could only figure out what was behind it all, we might have an important finding, an important discovery that pertained to an array of tumors, not just one tumor.”
In 1969, Drs. Li and Fraumeni submitted two papers that detailed the evidence for what they thought could be a familial syndrome. But without having an actual biological marker, they faced skepticism in the medical community. Their first paper was published in the Annals of Internal Medicine with a question mark in the subtitle.
“Fred was more conservative, more cautious, and more modest than I was. So, he insisted on putting in a subtitle with a question mark indicating the possibility that this could be a family syndrome. I took the question mark off. He put it back on, but he was right. He was more sensible.”
Over the next decade, the pair carefully followed up with the families. In 1982, they published a prospective study of the members of the original four families in which they found 16 new cases of cancer. By the late 1980s, Drs. Li and Fraumeni had identified 24 families with well-documented cases of the hereditary multicancer syndrome that became known as Li-Fraumeni syndrome. Those findings were published in the September 15, 1988, issue of Cancer Research, a journal of the American Association for Cancer Research (AACR).
But the two researchers had yet to identify a suspect—a specific gene that was passed down through these families, causing the syndrome. Luckily, they had stored blood samples from the family members whom they had studied, in hopes that future research would yield subsequent clues.
A suspect identified
Timing is everything. In the 1970s and 1980s the field of genetics was beginning to explode. Leading up to that time, the NCI had built a large program focused on viruses and cancer.
While researchers had viewed viruses as the chief culprit underlying cancer development, they had yet to decipher how certain viruses interacted with cellular components to cause cancer. In 1979, researchers including Drs. David Lane and Arnold Levine identified a protein that interacted with the cancer-causing SV40 and polyoma viruses. The size of the protein was 53 kilodaltons and was thus named p53.
In the years leading up to the identification of p53, researchers discovered that cancer could be caused by a patient’s genes going awry on their own. Oncogenes—genes that promote cancer when mutated or dysregulated—became a popular topic of research. Many scientists considered p53 an oncogene, but some of the data didn’t quite add up. In the mid-1970s, other researchers introduced the concept of tumor suppressor genes—genes that function to keep cell growth in check. Around the same time, the NCI sent Dr. Li to the Dana-Farber Cancer Institute to work in an NCI Field Station and continue studying the role of genetics in cancer.
“All these rapid developments, in laboratory research and in the areas of genetics, were occurring at the same time. And it took over the field of cancer causation,” said Dr. Fraumeni.
In 1989, geneticists reclassified p53 as a tumor suppressor that, when mutated or inactivated, leads to the development of cancer. This gave Drs. Li and Fraumeni an idea. What if the families with their inherited cancer syndrome were passing down defective copies of p53? In 1990, the pair, along with collaborators at Harvard and the MD Anderson Cancer Center, uncovered germline mutations in the p53 tumor suppressor gene in a group of families with the Li-Fraumeni syndrome.
“We had the hypothesis that was tested and shown to be correct with a finding that was seen in five consecutive families,” said Dr. Fraumeni.
A lasting legacy
The discovery marked a paradigm shift in the way the scientific community viewed cancer. While both lifestyle and environmental factors were still considered to be important, the role of genetic susceptibility in cancer causation was now firmly established thanks to the contributions of the two scientists. Researchers now recognize p53 as the most-commonly mutated gene in cancer and as a major driver of inherited cancer susceptibility.
“I think that the amount of research that is going on in p53 is incredible. It is mind-boggling. It is much more than any other gene that has been related to cancer, either in terms of cancer predisposition or in terms of cancer progression,” Dr. Fraumeni said.
The research of the two collaborators also played a major role in helping to launch the field of modern-day molecular epidemiology. At the time of Dr. Li’s death in 2015, he was revered as a pioneer in the field of cancer genetics.
“I never expected this amount of excitement having to deal with this syndrome in the work that we did,” said Dr. Fraumeni.
Throughout the pair’s quest for discovery, Drs. Li and Fraumeni were active members and leaders at the AACR. Both served on the AACR Board of Directors, were elected to the inaugural class of Fellows of the AACR Academy, and earned the AACR-ACS Award for Research Excellence in Cancer Epidemiology and Prevention, among others.
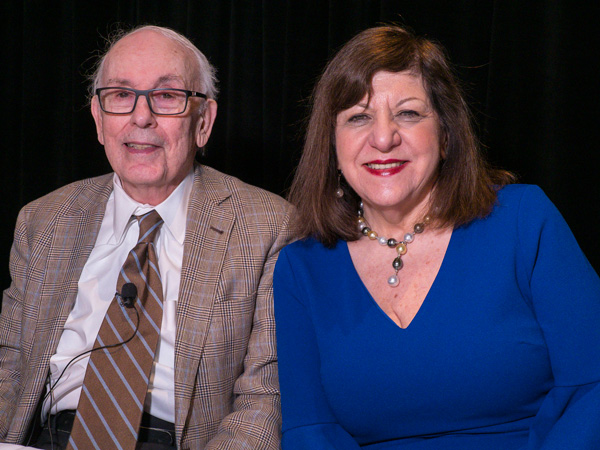
Dr. Fraumeni explained how the AACR, under the leadership of its Chief Executive Officer Margaret Foti, PhD, MD (h.c.), was a critical partner in bringing the field of molecular epidemiology to the forefront.
For example, Dr. Fraumeni noted that the AACR founded the Journal of Cancer Epidemiology, Biomarkers & Prevention in 1991. Dr. Li served as Editor-in-Chief of the journal from 1997 to 2002. Dr. Fraumeni went on to add that in 1999, Dr. Foti “created this new working group called Molecular Epidemiology, and that had a big impact. There were just a few people at first. But then it was just a really large group, a very active group.”
“I think that the impact of AACR has been enormous,” added Dr. Fraumeni. “All these conferences and workshops that the AACR hosts and fosters—it has been an important development. There really isn’t a meeting that doesn’t take place, that doesn’t have the fingerprints of the AACR on it.”
Return to AACR Stories Home