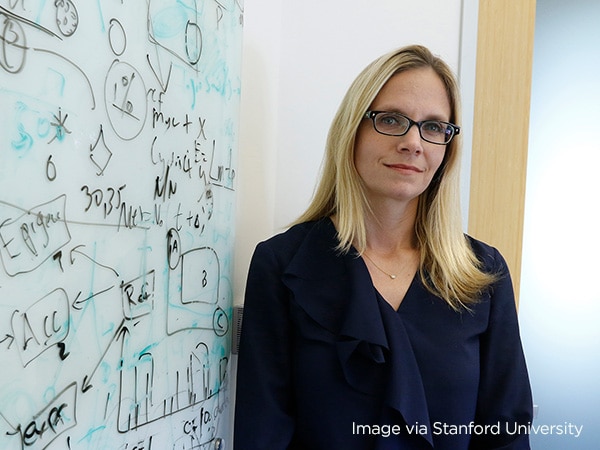
Christina Curtis, PhD, MSc: Researching Ways to Intercept Cancer at Its Earliest Stages
Tumors are “born to be bad” with metastatic potential present from the start, spreading to other organs when the original malignancy is the size of a poppy seed, she says.
As a teenager, Christina Curtis, PhD, MSc, knew that she wanted to study cancer and search for better ways to treat these devastating diseases. Having lost relatives to cancer, she wanted to know where cancer comes from and what could be done to lessen the impact on patients.
Today, Dr. Curtis is a professor of medicine at Stanford University and a renowned cancer researcher. After years of close study, she believes the best way to understand a tumor is to trace its growth and development—its evolution—back to its very earliest days, when it was just a tiny clump of cells, and see how it grows to the size at which it can be detected and identified.

In the past, the conventional explanation for tumor growth was that mutations occur in the genomes of individual cells, and the alterations that make the cell most fit become dominant and ‘sweep’ through the tumor. The process, which likely occurs in a stepwise fashion, also leaves many other mutations present in the tumor, accounting for the heterogeneity seen at later stages. Dr. Curtis’s research, some of which has been supported by AACR, suggests otherwise.
Based on a study of genomic data from colorectal cancer tumors, she and her colleagues proposed a different hypothesis about tumor evolution. The hypothesis, published in a 2015 paper, holds that, rather than picking up new mutations as it grows, the tumor consists predominantly of clones of the cells that were there at the beginning—a single expansion that carries along subclones of the primordial cells but muscles out new mutations.
“What you see in the final cancer was there from the beginning,” she says.
Dr. Curtis compares this hypothesis of tumor evolution to the reigning theory of the origin of the universe itself and calls it the “Big Bang” model.
“Several of our discoveries around how tumors evolve and how they metastasize actually afford clinical insights as well, because they tell us that some of the most critical events happen exceedingly early,” she said in an interview with AACR. “There’s actually potentially decades since the initiating hit, since the first mutation that gives us a real window of opportunity to ask, could we detect, could we intercept earlier? And moreover, can we risk-stratify patients who are really at risk of having a lethal tumor versus a more indolent tumor? … It’s a cause that I’m really committed to.”
A corollary of the “Big Bang” hypothesis is that the genetic mutations needed to drive the process of metastasis don’t come along late in the tumor’s development. Instead, they are acquired very early and start spreading the cancer to distant organs at an early point. Dr. Curtis estimates that up to 80 percent of colorectal cancers that have spread to other organs did so before the original tumor was bigger than a poppy seed.
She says that tumors like this —those malignancies packed with metastatic potential —are “born to be bad.”
In one of her studies, she found that cancer cells had already metastasized and begun to grow long before the primary tumor could be detected by standard diagnostic tools.
“This indicates that metastatic competence was attained very early after the birth of the cancer,” she said. “This runs counter to the prevailing assumption that metastasis occurs late in advanced primary tumors and has implications for patient stratification, therapeutic targeting, and earlier detection.” In other research, Dr. Curtis found evidence that this very early metastasis isn’t limited to colorectal cancer. In work funded in part by a grant from AACR, she found that very early seeding of metastatic cells occurs in lung and breast cancers as well.
“Metastatic seeding was estimated to occur 2–4 years before diagnosis of the primary tumor across three common cancer types, with breast cancers generally disseminating later and therefore closer to the time of detection relative to colorectal and lung cancers,” she and colleagues wrote in a paper published by Nature Genetics in 2020.
Scientists are still debating the “Big Bang” hypothesis versus the more traditional models of tumor growth. But the “Big Bang” shook up the field and was named by the Nature journals as a “Milestone in Cancer” during the first two decades of the century.
Dr. Curtis’ work was recognized by AACR with the 2022 Award for Outstanding Achievement in Basic Cancer Research. In 2009, she received a Scholar in Training award from AACR, and in 2016 she was awarded the AACR Triple-Negative Breast Cancer (TNBC) Foundation / Carol’s Crusade for a Cure Foundation Career Development Award. This is the grant she credits with helping her and her team look closely at metastasis in triple-negative breast cancer. She’s also grateful that AACR and its partners have been willing to take a chance on her research.
“Having funding from AACR has been huge,” she said. “A lot of this is a little bit out of the box. These are not your conventional approaches to tackling the problem. Sometimes more conventional funding mechanisms don’t expect to see that. So, it’s been great to have philanthropic support from AACR, to let us really go deep into these questions that I think are pertinent and timely. And from my perspective, we really need these answers now. We really need them sooner than later.”
Dr. Curtis feels her research fits well with the increasing emphasis on “interception” of cancer, the effort to detect and deal with precancerous conditions before they turn into identifiable cancers.
“We’re detecting malignancies much earlier,” she noted. “I think there is a huge opportunity for work in the early detection space. We know that we can better treat these tumors when we catch them earlier, and we’re developing noninvasive ways to do this.”
In addition to being an AACR grant recipient, she is also an enthusiastic supporter of the organization and has been involved in its work. She has served on the editorial board of AACR’s Cancer Discovery journal and serves on the AACR Board of Directors.
“AACR is really a guiding light for cancer research,” she says. “It helps set the stage and the tone for the most important initiatives and priorities. I think there have been tremendous examples of broad initiatives that have been rolled out through AACR.”
Although her research involves what is essentially looking backward in time, her view of the cancer research field looks very much to the future.
“There’s such a critical need for training, and I love it that part of AACR’s mission is to train the next generation,” she says. “There’s such a strong educational focus and also community building and mentorship, because we want to ensure that the next generation of bright minds are in tune to the most important questions in cancer research.”