The Curious Case of the Exceptional Responder
How Scientists Think Outside the Box to Unravel Cancer Mysteries
For decades, experimental cancer drugs that did not provide measurable benefit to a significant number of patients in a clinical trial were considered “failed,” and further efforts to develop the drug for that use were shelved. The few patients who responded to such drugs were thought to have experienced a “miracle.”
In recent years, focus has shifted toward those exceptional responders, the fortunate few who benefited from otherwise unsuccessful clinical trials. Thanks to genomic sequencing – a recent, paradigm-shifting technology that enables complete sequencing of the tumor exome and identification of almost all of the genetic alterations – cancer clinicians and scientists could tap into this treasure trove to track down genetic alterations responsible for the exceptional responses in their patients.
This is how, for example, Nikhil Wagle, MD, an instructor in medicine at the Dana-Farber Cancer Institute, was able to decipher how a bladder cancer patient of his had an exceptional and complete response for 14 months to the drug combination everolimus and pazopanib in a phase I trial that did not benefit most other patients. Wagle and colleagues performed whole-exome sequencing of the patient’s tumor and identified two mutations that activated the mTOR-mediated signaling pathway. Functional assessment suggested that these mutations likely rendered the patient’s cancer dependent on the mTOR pathway to survive, forcing his cancer to succumb to the mTOR inhibitor everolimus.
“This study is yet another example of how therapies targeted toward the genetic features of a tumor can be highly effective, and our goal moving forward is to be able to identify as many of these genetic features as possible and have as many drugs that target these genetic features as possible, so we can match the drugs to the patients,” said Wagle, in a news release on this study published in Cancer Discovery, a journal of the American Association for Cancer Research.
To that end, the National Cancer Institute is about to launch two new initiatives, the Exceptional Responders Initiative, which will identify tumor targets in exceptional responders of unsuccessful phase II trials; and the MATCH trial, which will match molecularly-informed targeted therapies to patients with unresponsive tumors. Together, these initiatives will help tackle the challenges of finding the right kind of treatment to the right patient.
As we step into the era of precision medicine, it is becoming increasingly clear that knowledge of the genetic alterations that drive cancers of diverse origins will permit better-informed treatment options. After all, in this day and age, where everything from cellphones to news is personalized to suit individuals’ palates, it makes perfect sense to manage cancer, a disease that is unique to each patient, with tailored treatment regimens rather than conventional, less-precise approaches.
As scientists find new ways of putting pieces of the cancer puzzle together, we can all hope for exciting times in cancer research and treatment where every cancer patient will have an exceptional response.
Cover photo: “DNA orbit animated static thumb” by Zephyris is licensed under CC BY-SA 3.0


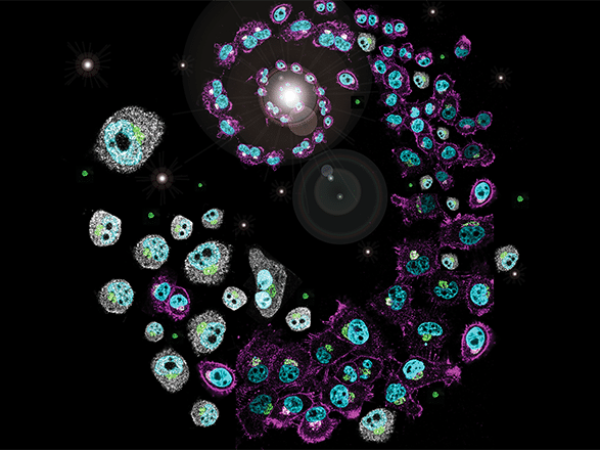
Exome sequencing can pinpoint mutational differences of the signaling protein between normal cells and cancerous counterparts. Targeting a drug to the mutant protein which alters the signaling pathway sounds viable theoretically but how do you target a drug to a heterogenous tumor?