Lung Cancer Progress Made, But We’re Not There Yet
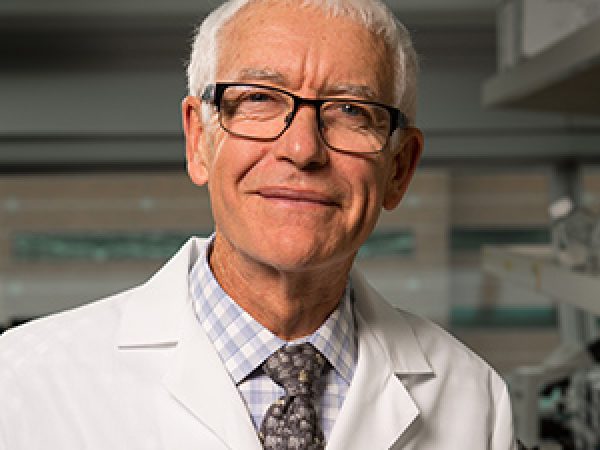
Guest Post By Fadlo R. Khuri, MD
Winship Cancer Institute of Emory University
Luther Terry, the ninth Surgeon General of the United States, released his now seminal Smoking and Health: Report of the Advisory Committee to the Surgeon General of the United States on Jan. 11, 1964. The report, assembled by a brave and committed panel of independent physicians and scientists, definitively concluded that lung cancer and chronic bronchitis are causally related to cigarette smoking.
Fifty years later, genomic discovery and the rapidly accelerating fields of epigenetics, proteomics, metabolomics, and drug discovery have presented an armada of new options for patients with lung cancer. CT screening of high-risk individuals, particularly smokers, helps detect the disease in its early, more-curable stages more than 80 percent of the time. Breakthroughs in cancer immunology have led to the accelerated development of PD-1 and PD-L1 inhibitors, demonstrating remarkable and durable benefits in early clinical trials of lung cancer patients with advanced disease. But in 2014, five-year survival remains under 20 percent for patients diagnosed with lung cancer and more than 1.5 million people worldwide will die of lung cancer. Moreover, smoking rates, while down to 19 percent in the U.S., remain well over 30 percent in much of the rest of the world.
Despite the armada of new targeted medicines, cure remains elusive for the vast majority of patients diagnosed with this dreaded illness, and a significant number of never-smokers seem to contract this disease without any known risk factors. So why are we optimistic that major progress made in science can meaningfully impact lung cancer?
2014 has seen major strides in lung cancer research and treatment. Smoking cessation efforts have accelerated with the Food and Drug Administration’s increased abilities to enforce regulations on tobacco products. Our understanding of lung cancer biology grows exponentially by the day. A number of exciting trials have been launched this year to test targeted agents in the adjuvant, postoperative setting, as well for therapy of patients with advanced stage disease. Exciting clinical trials have led to the approval of second- and third-generation agents targeting oncogene-driven tumors. A major initiative has been launched to target RAS, the most frequently mutated oncogene in all cancer, and a major driver of outcomes in lung cancer.
Substantial progress has been achieved this year in targeted therapy, stereotactic radiation, and immunotherapy of lung cancer. Collaborative work demonstrated that patients with metastatic lung cancer who were treated successfully by targeting their oncogenic drivers do better than individuals who were treated with standard approaches across several centers of excellence, and that work needs to be successfully translated in the community for all patients with lung cancer in the coming years. While emergence of resistance, triggered through enhanced survival signaling circuits, is inevitable in these highly complex tumors, our understanding of these escape circuits is accelerating rapidly. We are learning to combine improved imaging methods with superior technology to detect circulating tumor cells in order to identify and treat patients with disease earlier than ever before.
However, we have yet to show we can successfully intervene in lung carcinogenesis. In a large trial that we performed in the ECOG-ACRIN Cancer Research Group, we found that natural compounds are incapable of reversing the damage caused by ongoing tobacco smoke. We must ally smoking cessation and early detection, and enhance our understanding of the cause of disease in never-smokers. We need to develop potent but tolerable compounds that can reverse premalignant lesions in former smokers.
While the 2009 Tobacco Control Act has enhanced the FDA’s ability to regulate tobacco products in some key areas, such as marketing to minors, major obstacles regarding the regulation of cigars, water pipes, menthol, and particularly e-cigarettes have limited the FDA’s ability to more effectively regulate the menace of Big Tobacco. Indeed, the booming electronic cigarettes industry threatens to enable a whole new generation of smokers. Unless we act decisively to carefully regulate the use of e-cigarettes, the steady progress made in lung cancer research and therapy over the past few decades could be eroded. It is only when we effectively reduce smoking by enforcing the FDA’s control of all products and implementing tobacco control programs with real teeth while simultaneously unraveling and preventing the causes of lung cancer in never-smokers that we will truly start to make an impact, fulfilling Surgeon General Terry’s and, most importantly, our patients’ goals to make lung cancer a disease of prior generations, and a scourge no more.
Fadlo R. Khuri, MD, serves as Deputy Director for the Winship Cancer Institute of Emory University in Atlanta. He is professor and chairman of the Department of Hematology & Medical Oncology, Emory University School of Medicine. Khuri holds the Roberto C. Goizueta Distinguished Chair for Cancer Research. He is a professor of otolaryngology, medicine, and pharmacology, and he also serves as editor-in-chief of the journal Cancer. Khuri is considered one of the leading translational clinical investigators and physicians in lung and aerodigestive medical oncology in the world.
Khuri has been a member of the AACR for 21 years. He received the 37th Annual AACR-Richard and Hinda Rosenthal Memorial Award in recognition of his accomplishments as an investigator in lung and aerodigestive medical oncology at the AACR Annual Meeting 2013 and is a member of the AACR Tobacco and Cancer Subcommittee.



amazing article…would love see more information on lung cancer treatment
Hi, thank you for your comment! Here are a few of our recent blog posts on advances in lung cancer treatment.
http://blog.aacr.org/advancing-lung-cancer-research/
http://blog.aacr.org/fda-approval-liquid-biopsy-test-lung-cancer/
http://blog.aacr.org/fda-approves-new-immunotherapy-option-lung-cancer/
Smoking is bad for smokers’ health and also for the persons who are living with the smokers. Smoking is harmful for both smokers as well as non-smokers. Smoking gives much disease. Smoking should be banned in outdoor seating areas.