Q&A With Elaine R. Mardis, PhD, on Integrating Clinical Genomics and Cancer Therapy
As we witness the convergence of advancements in genomic sequencing technologies, evidence-based improvements in targeted therapies, and a growing recognition of the need for noninvasive methods to diagnose and monitor disease, the AACR is excited to host its third conference in the Precision Medicine Series, “Integrating Clinical Genomics and Cancer Therapy,” in Salt Lake City, Utah, June 13 to 16.
Precision medicine, the tailoring of disease prevention and treatment based on the characteristics of each individual, is rapidly becoming one of the mainstays of cancer management, largely due to technological advancements and our increasing understanding of the disease. Last week, the National Cancer Institute launched the Molecular Analysis for Therapy Choice Program (MATCH) trial, in which patients’ tumors will be studied to determine whether they contain genetic abnormalities for which a targeted drug exists and assign treatments based on the abnormalities. The MATCH initiative is complementary to the Precision Medicine Initiative proposed by President Obama, which has the goal of considering individual differences in people’s genes, environments, and lifestyles to prevent and treat diseases, including cancer.
The AACR has been at the forefront of providing platforms for experts in precision medicine to meet and interact, and to help them make significant progress in the field. In 2013, the AACR introduced the Precision Medicine Series to highlight the incredible technological advances in cancer research that are enabling treatments precisely targeted to the unique molecular and genetic characteristics of an individual’s cancer. The focus of the third conference in the series is on the rapid advances made in clinical genomics, integrated DNA and RNA analysis, and the management and operability of these critical data for cancer therapy.
I spoke with conference co-chair Elaine R. Mardis, PhD, director of the McDonnell Genome Institute at the Washington University School of Medicine, to provide insight into the important, transformative studies to be presented at the meeting, and asked for her expert opinion on the impact of precision medicine in the near and distant future of cancer treatments. Read on and watch this video, compiled by our colleagues at the Siteman Cancer Center at the Barnes-Jewish Hospital and Washington University School of Medicine, for her thoughts.
https://www.youtube.com/watch?v=DA-ocApDEI8
“Integrating Clinical Genomics and Cancer Therapy” is the third conference in the AACR’s Precision Medicine Series. What prompted the selection of this topic for the 2015 meeting?
The increasing applicability of massively parallel sequencing to make fundamental discoveries about the drivers of tumors has enabled the convergence of cancer genomics and targeted therapy quite recently. Initiatives at the Memorial Sloan Kettering Cancer Center led by conference co-chair Charles Sawyers, MD, to increase the use of massively parallel sequencing to look at each and every cancer patient’s tumor in their clinics; the long-standing and successful molecular tumor boards for the implementation of precision medicine in cancer care initiated by conference co-chair and University of Michigan Comprehensive Cancer Center pathologist Arul Chinnaiyan, MD, PhD; and the initiatives made by my team at the McDonnell Genome Institute toward applying next-generation sequencing to support therapeutic decision-making prompted us to get experts together to represent everything that’s going on in this space.
What role has the AACR played, and what role will it continue to play, in impacting the field of precision medicine?
This is the third meeting in the AACR’s Precision Medicine Series. The first, in 2013, was “Synthetic Lethal Approaches to Cancer Vulnerabilities” and the second, in 2014, which I helped organize, was “Drug Sensitivity and Resistance: Improving Cancer Therapy.” You can see that the AACR has been consistently providing excellent forums, like the one that’s about to take place in Salt Lake City, to enable experts to get together and hear about what’s latest in this area. The AACR makes every effort to help attendees ask probing questions about what’s easy and what’s hard about making all of this work in a clinical environment.
What advances have been made recently in managing big data and data interpretation?
Recent focus has been on turning big data into meaningful, clinically usable information to physicians and patients in a reasonable time frame. We are starting to see an emergence of some very clever approaches of bioinformatics that can analyze complex data sets in a timely manner and in an interpretable fashion. I do think we still have a lot of work to do in terms of training existing licensed and practicing clinicians, oncologists, pathologists, and other medical professionals in these new methods and identifying effective methods in incorporating them into evidence-based medicine. We do have some challenges, both in terms of expertise and cost-effectiveness, in applying advanced techniques to everyday clinics.
Recent focus has been on turning big data into meaningful, clinically usable information to physicians and patients in a reasonable timeframe.
Can you tell us what you think are likely to be the top breakthroughs to be reported at this meeting?
I think we will see important information emerging on how well the use of genomic sequencing is leading to effectively bringing targeted therapy to patients. There will be some presentations that highlight the logistics and setbacks of getting an appropriate targeted therapy for a patient whose tumor is sequenced and has a clearly targetable lesion. I think the other area that’s emerging and we will hear a lot about is the availability of decision support tools, such as what is needed for clinicians and patients to access information and how to use it intelligently. Lastly, I’m hoping to hear more about the use of genomics in the spectrum of immunotherapy because there are some emerging data sets in predicting cancer-immunotherapy response.
What were the criteria in selecting abstracts for oral presentations?
It is a combination of two things: one, responsiveness to the theme of the meeting; and two, we try to encourage younger scientists doing brilliant research who may not necessarily be from the larger, tertiary-care hospital settings. I think that’s a fairly common theme throughout the AACR special conferences. It is always refreshing to get these younger scientists up on the platform and hear what they have to say because in many cases, they present remarkable results that I think are very informative to everyone and it gives them a chance to shine as well.
We try to encourage younger scientists doing brilliant research who may not necessarily be from the larger, tertiary-care hospital settings. I think that’s a fairly common theme throughout the AACR special conferences.
Could you please preview some of the important presentations to be made at the conference?
An “N of 1” exceptional responder study features a precision medicine clinical research protocol for pediatric, adolescent, and young adult cancer patients, with the goal of making genome-informed treatment recommendations in a clinically relevant time frame. I am intrigued by this because there haven’t been many reports on N-of -1 study in pediatric patients that I am aware of, so I think that’ll be an eye-opener.
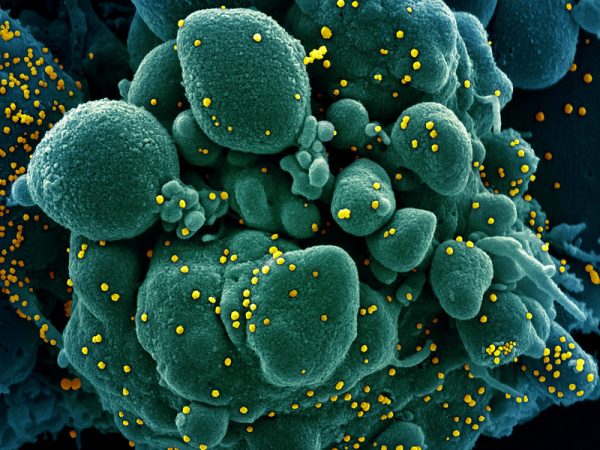
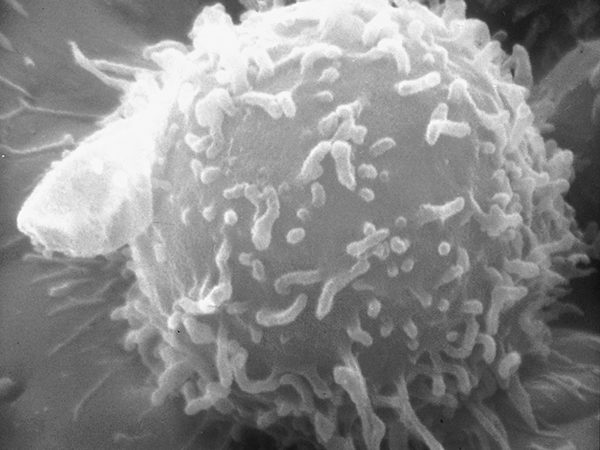
There is an interesting presentation on personalized vaccines that uses genomic sequencing of the patient’s tumor to identify neo-antigens and use them in vaccine design. A presentation by the Personalized OncoGenomics (POG) project launched by the British Columbia Cancer Agency, which uses genome analyses to support cancer treatment decision making, will discuss how they integrated genomic sequencing and bioinformatics to build individual somatic molecular profiles, and performed intensive pathway analysis and literature searches to identify deregulated biological processes and therapeutic options based on this integrated approach.
We have a whole session on another hot area that is highly relevant to the application of targeted therapy and disease monitoring, which is sequencing of circulating single cells – I’m very excited about this one. There is a presentation on the application of plasma-Seq, a method to sequence circulating DNA (ctDNA) in the blood of cancer patients, to help identify the occurrence of novel changes associated with resistance to therapy in castration-resistant prostate cancer.
There are a lot of clinical trials now that focus on using blood-based monitoring to track progression of the disease in patients whose cancers have become resistant to therapies. To me, this is one of the most exciting interfaces between genomics and clinical application because tumor biopsies are very, very hard to come by, and generating high-quality genetic material to work with adds another level of complexity. So the surrogacy through liquid biopsy approach, I think, is very promising and we’ll get to see some nice examples in this session.
What are the most exciting areas of precision medicine to look for, moving forward?
It is certainly the liquid biopsy that we just talked about, and I think the other big thing is going to be immunotherapy and targeted therapy coming together. There are groups that are trying clever mechanisms of tying together a short-term treatment with targeted therapy to reduce the tumor burden, followed by immunotherapy to make the response more durable. To me, that’s really where the more bang for your buck is —in getting patients to a point where they’re feeling better, but can also continue to feel better for a long time. If we can successfully incorporate liquid biopsy to consistently monitor patients who have received such combination therapies, we would have a beautiful synthesis of all these different fields coming together to translate genomics into the next level of cancer care.