Overcoming Drug Resistance: The EGFR Enigma
Editor’s note: Cancer researchers from around the world will convene in Florence, Italy this weekend to discuss the development of targeted therapies and strategies to overcome resistance to these therapies. Learn more about the EACR-AACR-SIC Special Conference on Anticancer Drug Action and Drug Resistance: From Cancer Biology to the Clinic.
Part 1: Overcoming Resistance to EGFR TKIs
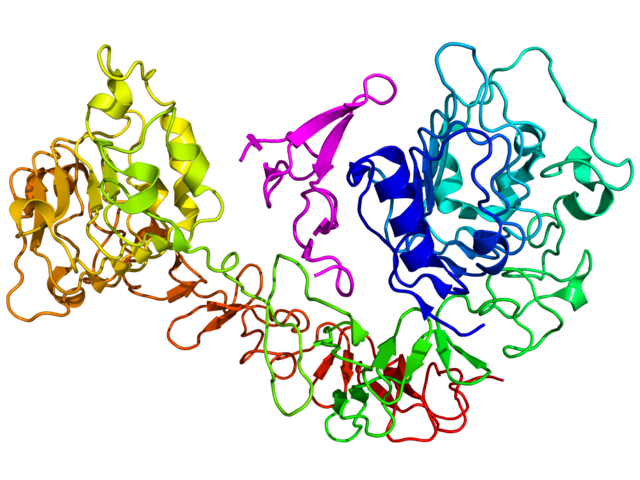
There are some molecular targets in cancer that continue to elude cancer researchers as they pose many challenges with druggability. The epidermal growth factor receptor (EGFR) is not one of them. Following its discovery, researchers gained a fairly good understanding of its role in promoting many solid tumors. Several drugs targeting this receptor have been developed, such as the U.S. Food and Drug Administration-approved first-generation EGFR tyrosine kinase inhibitors (TKIs) gefitinib (Iressa) and erlotinib (Tarceva); the second-generation TKIs, such as the FDA-approved afatinib (Gilotrif) and the investigational drugs neratinib and dacomitinib; and the FDA-approved anti-EGFR monoclonal antibody therapies cetuximab (Erbitux) and panitumumab (Vectibix).
Currently, anti-EGFR therapies are approved by the FDA for the treatment of non-small cell lung cancer (erlotinib and afatinib), squamous cell carcinoma of the head and neck (cetuximab), pancreatic cancer (erlotinib), and colorectal cancer (cetuximab and panitumumab).
Most patients receiving anti-EGFR therapies benefit from the treatment, but the challenge they face, as do patients receiving most other targeted therapies, is that their tumors ultimately develop drug resistance. So efforts are underway to develop newer anti-EGFR therapies that can circumvent resistance to existing EGFR inhibitors.
A series of peer-reviewed papers published in the AACR journals Clinical Cancer Research and Cancer Discovery have dissected the mechanisms of resistance to anti-EGFR therapies and investigated different approaches to outsmarting drug resistance.
In this post, I discuss two studies that address the challenges with overcoming resistance to EGFR TKIs. In my next post, I will discuss some studies that tested first-in-class drugs in clinical trials to overcome resistance to EGFR-specific antibody therapies.
Tackling the T790M Challenge
The most frequent activating EGFR mutations in non-small cell lung cancers include the exon 19 deletion and L858R. Patients whose tumors harbor such activating EGFR mutations are treated with first-generation EGFR TKIs with reasonable success; however, about 60 percent of these tumors acquire a “gatekeeper” point mutation called T790M, which interferes with the ability of these drugs to bind to the EGFR and enables activation of alternate signaling pathways. This led to the development of second-generation EGFR TKIs, which form irreversible bonds with the target to achieve prolonged effectiveness. However, clinical trials have shown that many second-generation EGFR TKIs inhibit both mutant and wild-type (normal) EGFR, which make them toxic to normal cells at the doses required to inhibit mutant EGFR. As a result, third-generation TKIs are being developed, such as AZD9291 and CO-1686, which are more selective to both the activating EGFR mutations and the acquired T790M mutation while sparing wild-type EGFR, potentially making them more specific and less toxic.
The Scope of Third-generation EGFR TKIs
In a couple of studies, researchers conducted elegant laboratory experiments to show that mutated lung cancer cells find ways to develop resistance to the third-generation EGFR TKIs as well. Their studies provide valuable insights into the mechanisms of resistance and potential ways to devise treatment strategies with existing drugs.
In a study published in Clinical Cancer Research, investigators tested the third-generation EGFR TKIs on lung cancer cells harboring the T790M mutation derived from an erlotinib-resistant tumor, and identified yet another mutation, C797S, which conferred resistance to third-generation TKIs. The authors found that depending on which EGFR allele the two mutations (T790M and C797S) are located, it may be possible to derive benefit from TKIs of different generations. For example, lung cancers that have the two mutations on different alleles may respond to a combination of first- and third-generation TKIs; however if the mutations are on the same allele, such cancers may not respond to any TKI, either alone or in combination. The authors have concluded that it is important to sequence for C797S mutation in patients with acquired resistance to third-generation TKIs to determine further treatment strategies.
In another study, which also appeared in Clinical Cancer Research, researchers used cells harboring the T790M mutation and identified three EGFR mutations, EGFR L718Q, L844V, and C797S, which mediated resistance to the third-generation EGFR TKIs CO-1686 and WZ4002; only C797S caused resistance to AZD9291. Here again, the authors have described some genomic contexts—combinations of activating and acquired mutations—in which the cancers may not respond to any of the existing TKIs, and some contexts in which they may remain sensitive to some TKIs.
Understanding and anticipating the responses to third-generation EGFR TKIs, as these studies have done, are instrumental in guiding the development of new treatment strategies for patients with EGFR-mutant non-small cell lung cancer.