Advances in Immunotherapy: Fine-tuning CAR T Cells
Two teams tinker with the target-binding end of CAR T cells to make them safe for patients with solid tumors
Enlisting components of our immune system to attack cancer cells, the principle behind immunotherapy, has been approached in a number of different ways. One approach, discussed extensively on this blog, involves blocking the PD-1/PD-L1 pathway using immune-checkpoint inhibitors, which unleashes immune cells called T cells so they can attack cancer cells. Another approach, called adoptive T-cell transfer, is the technology behind CAR T-cell therapy, which involves removing T cells from a patient’s body, modifying them so that they can recognize the patient’s tumor cells, and reintroducing them in to patient’s body where the “equipped” T cells multiply and attack cancer cells.
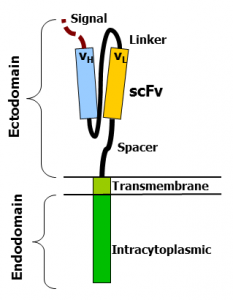
A key step in CAR T-cell therapy is to genetically modify the T cells removed from the patients’ body—a step in which a CAR, short for chimeric antigen receptor, is introduced to the T cell. The CAR has three distinct regions—the antigen-binding ectodomain, which includes a single-chain variable fragment (scFv) that is developed using monoclonal antibodies to recognize the target protein on the cancer cell; the T-cell signaling endodomain, which transmits a signal to the T cell once the svFv recognizes a cancer cell; and a transmembrane domain, the segment in between the ecto- and endodomain that anchors the CAR to the T cell. Significant improvements have been made to the endodomain by adding multiple co-stimulatory signaling molecules (resulting in second- and third-generation CAR T cells) to increase CAR T-cell efficiency.
CAR T-cell therapy works well for B-cell malignancies, but what about solid tumors?
Third-generation CAR T cells that target a protein called CD19 present in cancerous B cells (and most normal B cells) are currently being tested as treatments for some forms of leukemia and lymphoma. Data from three CD19 CAR T-cell clinical trials, the CHOP trial, the POB trial, and the MSKCC trial, showed promising outcomes for patients with some forms of leukemia, with up to 90 percent of the patients experiencing complete response.
CAR T cells designed to target CD19 in B-cell cancers are not selective. They cannot distinguish cancerous B cells that have high levels of CD19 from normal B cells that have physiological (lower) levels of the same protein. But this does not severely impede treating B-cell malignancies because a patient’s immune system can function even when normal B cells are depleted. This form of immunotherapy, however, is not readily adaptable to solid tumors because targetable proteins present on the cancer cells of solid tumors, such as ErbB2 and EGFR, are also present on normal cells that form the vital organs of the body. While losing normal B cells when treated with CD19 CAR T-cell therapy poses manageable side effects in a patient, loss of normal cells that are part of vital organs when treating solid tumors with CAR T-cell therapy can damage these vital organs, which has serious consequences. In fact, in a case report, CAR T cells designed to target ErbB2 present in metastatic colon cancer cells also attacked cells in the patient’s lungs that had low levels of ErbB2, resulting in severe toxicity and death. So, it became evident that if CAR T-cell therapy were to work for solid tumors, engineering T cells that can selectively target cancer cells and spare normal cells is inevitable.
The two teams
Enter scientists from the University of Pennsylvania and The University of Texas MD Anderson Cancer Center, two teams that used different approaches to answer the same question: Will lowering the affinity of CAR T cells to the target protein make them selective to cancer cells that have high levels of the protein and spare normal cells that have low levels of the same protein?
Based on the data the two teams published independently in the AACR’s journal Cancer Research, it appears the answer is “Yes.”
Low-affinity CAR T cells targeting ErbB2
A team of scientists in the laboratory of Carl June, MD, director of the University of Pennsylvania’s Center for Cellular Immunotherapies, including Yangbing Zhao, MD, PhD, director of the T-Cell Engineering Laboratory (TCEL) at the center, have been working for the past couple of years to optimize a system to fine-tune the affinity of the target-binding scFv segment in a CAR T cell. They hypothesized that lowering the affinity of CAR T cells could make them only recognize (cancer) cells that have high levels of the target and not have the ability to recognize (normal) cells that have low levels of the same protein. The target protein they chose was ErbB2, which is often overexpressed in breast cancer, and is also present at low levels in normal cells, including heart and lung cells.
Using previously published sequencing data on varying affinities of 4D5 antibodies to ErbB2, Zhao and colleagues first engineered a panel of scFvs with varying affinities to ErbB2. They then incorporated different scFvs into the CAR backbone, such that they generated CAR T cells with a range of affinities for ErbB2. In fact, the newly engineered CAR T cells varied in their affinity to ErbB2 by three orders of magnitude.
After conducting a series of experiments using cancer cells that have high levels of ErbB2 and non-cancer cells that have low levels of the protein, in cell cultures and in animals, the team concluded in their paper that the low-affinity ErbB2-directed CAR T cells were able to selectively target cancer cells and spare normal cells.
“Unlike the common expectation that lowering the affinity of CAR T cells might also lower their efficacy, we have shown that lowering the affinity in fact does the opposite—lower-affinity CAR T cells displayed more potent reactivity to tumor cells expressing high levels of the target than did higher-affinity CAR T cells,” Zhao said in an interview.
Low-affinity CAR T cells targeting EGFR
Around the same time, another team at The University of Texas MD Anderson Cancer Center, led by Laurence Cooper, MD, PhD, a professor of pediatrics at the center at the time of this study and presently CEO of ZIOPHARM Oncology, were working on the same challenge. “The goal of [our] study was to make CAR-expressing T cells differentiate friend from foe,” Cooper said in an interview. The protein target Cooper and colleagues chose was EGFR, a protein present in high quantities in certain brain cancers and in low levels in normal cells, including cells of the skin, kidney, and gastrointestinal tissue.
The researchers used two monoclonal antibodies—cetuximab, which has higher affinity for EGFR, and nimotuzumab, which has lower affinity for EGFR—and engineered scFvs to develop high-affinity CAR T cells (cetux-CAR T cells) and low-affinity CAR T cells (nimo-CAR T cells). Experiments to test these engineered T cells showed that unlike the cetux-CAR T cells, low-affinity nimo-CAR T cells had the ability to selectively target cancer cells and spare normal cells.
This technology could be used to develop CAR T cells that can be fine-tuned to target other overexpressed cancer proteins besides EGFR, Cooper explained. “An important derivative of this study is that scientists can now tweak, or modulate, the affinity of a CAR T cell to meet the needs of a given tumor.”
Both studies have proven that safer, more potent CAR T cells developed by fine-tuning scFvs is a promising next step in bringing CAR T-cell therapies to solid tumor treatment arena. It will be exciting to watch the progress these teams make.