FDA Approves First Immunotherapy-Companion Diagnostic Combo for Lung Cancer
On the heels of the U.S. Food and Drug Administration’s approval of a combination of immune checkpoint inhibitors for unresectable and metastatic melanoma comes yet another immunotherapy approval. This time it is pembrolizumab (Keytruda), an immune checkpoint inhibitor, being approved for patients with metastatic non-small cell lung cancer (NSCLC) that has progressed after other treatments, and whose tumors express the protein PD-L1.
This is the first immunotherapeutic to be approved in conjunction with a companion diagnostic test, the PD-L1 IHC 22C3 pharmDx test, which can detect the presence of the protein PD-L1 in non-small cell lung tumors.
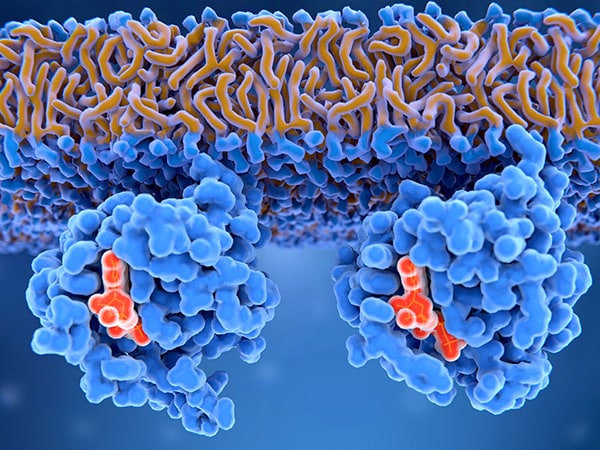
Pembrolizumab is the second drug in the class of immune checkpoint inhibitors to be approved for NSCLC, the first being nivolumab, which was approved for treating squamous NSCLC in March this year. Pembrolizumab works by blocking the PD-1/PD-L1 pathway that cancer cells sometimes engage in order to apply “brakes” on cancer-fighting T cells, preventing the T cells from doing their job. Blocking the PD-1/PD-L1 pathway releases the brakes on T cells and enables them to fight cancer cells.
The FDA’s approval is based on the results of a randomized clinical trial of 550 patients with advanced NSCLC. In a subgroup of patients who received pembrolizumab after their lung cancer progressed following chemotherapy or targeted therapy and whose tumors had PD-L1, the overall response rate was 41 percent, and the treatment effect lasted between 2.1 and 9.1 months.
Early results from this trial were presented in April at the AACR Annual Meeting 2015. At that time, describing the promising data from the study, Edward B. Garon, MD, associate professor of medicine at the David Geffen School of Medicine at the University of California, Los Angeles, said in a press release, “Neither the drug nor the biomarker test is approved for use in this setting at this time, but if I had a patient whose tumor had PD-L1 expression on at least half of the cells and if pembrolizumab was available, I think that I would find the data compelling to look at the drug as the treatment option for that patient.” The results of this study were published in the New England Journal of Medicine.
The Diagnostic Tests Dilemma
While immune checkpoint inhibitors are one of the most promising classes of drugs to be tested and approved in recent years, their use is not without challenges.
As individual pharmaceutical companies continue to develop diagnostic tests to identify patients most likely to benefit from the immune checkpoint inhibitor they are each developing, and as more and more therapeutics from this class of drugs are approved by the FDA for a range of cancer types, identifying the right drug in a reasonable timeframe and making it a cost-effective endeavor poses challenges for both the patient and his or her physician.
Recognizing the challenges and in an effort to develop some solutions, the FDA, the AACR, and the American Society of Clinical Oncology (ASCO) held a one-day workshop in March this year in Washington, D.C., titled “Complexities in Personalized Medicine: Harmonizing Companion Diagnostics across a Class of Targeted Therapies.”
A significant development to emerge from the workshop was a commitment from six companies to work together in the pre-competitive space and analytically characterize the performance of their individual PD-1/PD-L1 companion diagnostic test systems. The project is continuing to make strides, and results are expected to help build an evidence base for post-approval studies that will help inform patients, physicians, pathologists, and others on how best to use the tests to determine treatment decisions.