FDA Approves First Liquid Biopsy Test for Lung Cancer Patients
On June 1, the U.S. Food and Drug Administration (FDA) approved a liquid biopsy test, a companion diagnostic test called cobas EGFR Mutation Test v2. The test uses plasma samples to identify patients with metastatic non-small cell lung cancer (NSCLC) eligible for treatment with the EGFR-targeted therapeutic erlotinib (Tarceva).
The test detects specific alterations in the gene epidermal growth factor receptor (EGFR): exon 19 deletions or exon 21 (L858R) substitution mutations. These mutations are present in about 10 to 20 percent of NSCLCs, the most common type of lung cancer.
This is the first liquid biopsy test approved for use by the FDA.
What is a liquid biopsy?
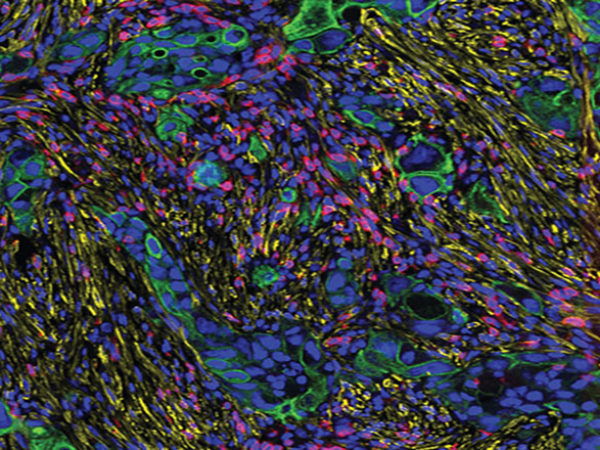
Unlike a traditional biopsy—an invasive procedure to collect a piece of the tumor tissue that requires local anesthesia, causes discomfort to the patient, and may not always be feasible because of the location of the tumor or several other reasons—a liquid biopsy is essentially a blood draw. The blood samples are spun down to collect plasma and isolate DNA shed by the tumor into blood circulation, so called circulating-free tumor DNA (CfDNA).
 Advanced technologies have now made it possible to analyze small amounts of cfDNA for mutations pertaining to a specific disease. In the case of this newly approved test, the cfDNA is analyzed for the presence of the specific mutations in the EGFR gene, the presence of which make the patients eligible for treatment with the FDA-approved drug erlotinib.
Advanced technologies have now made it possible to analyze small amounts of cfDNA for mutations pertaining to a specific disease. In the case of this newly approved test, the cfDNA is analyzed for the presence of the specific mutations in the EGFR gene, the presence of which make the patients eligible for treatment with the FDA-approved drug erlotinib.
The ease with which liquid biopsies can be obtained makes them also useful in real-time monitoring of disease progression because, in many cases, tumors evolve and may need different treatments based on the genetic changes that occur within the tumor.
What was the basis for this approval?
The FDA previously approved the cobas EGFR Mutation Test to detect EGFR mutations in formalin fixed, paraffin embedded (FFPE) tumor samples obtained through a biopsy. In order to determine whether this test can be used on liquid biopsy samples, researchers compared test results obtained from FFPE samples with those from liquid biopsy samples in a clinical trial: In a multicenter, phase III trial researchers compared the efficacy of erlotinib as first-line therapy with that of a combination of the chemotherapies, gemcitabine and cisplatin, in patients with late-stage NSCLC. All patients had their tumor tissue specimens tested for the EGFR exon 19 deletion or L858R mutations, as determined by the cobas EGFR Mutation Test. Of those enrolled, 98.6 percent had plasma samples available, which were used to detect the mutations using the cobas test.
Of the tissue samples that were positive for the specific EGFR mutations, 76.7 percent of the corresponding plasma samples also showed positive results for the test; of the tissue samples that were negative for the specific EGFR mutations, 98.2 percent of the corresponding plasma samples also showed negative results for the test.
Becoming the new standard of care
In an interview to forecast cancer research and treatment advances in 2016, a precision medicine expert at Memorial Sloan Kettering Cancer Center, David Solit, MD, said, “The use of circulating free DNA collected from blood [liquid biopsy] to determine which treatment a cancer patient should receive is already a reality, and will begin to change the way we diagnose and treat patients in 2016. In 2016 and 2017, we will likely see liquid biopsies becoming a standard of care for some cancer types.”
In May, the AACR’s journal Molecular Cancer Therapeutics published a study in which researchers at The University of Texas MD Anderson Cancer Center developed a PCR-based liquid-biopsy test called IdyllaTM BRAF Mutation Test, which they found to be feasible and concordant with standard tests of archival tumor biopsy samples of advanced cancers. The test has a short turnaround time of 90 minutes. The test detects BRAF V600 mutations, which are commonly present in colorectal cancer and melanoma, but also in several other cancers, and FDA-approved targeted therapies are available to treat cancers with such BRAF mutations.
The researchers found that the liquid biopsy test had 88 percent concordance with results from the standard tests that used paraffin-embedded tissues, in samples collected at baseline. The concordance was 90 percent when results from samples collected at any time point during the course of the treatment were compared. They also found that the amount of BRAF V600 mutant cell-free DNA, as detected by the Idylla system, was predictive of the overall survival of the patients.
With FDA approvals and studies such as these, as Solit predicted, we are truly moving toward making cancer diagnosis and treatment monitoring a more efficient and convenient endeavor to cancer patients in the near future.