Ibrutinib Use Expanded to Additional Type of Non-Hodgkin Lymphoma
Last week, the U.S. Food and Drug Administration (FDA) approved expanding the use of the molecularly targeted therapeutic ibrutinib (Imbruvica) to include the treatment of certain patients with a type of non-Hodgkin lymphoma called marginal zone lymphoma. Specifically, the FDA approved ibrutinib for treating patients with marginal zone lymphoma that has progressed despite treatment with at least one CD20-targeted therapeutic.
With this decision, ibrutinib is now approved for treating three types of non-Hodgkin lymphoma—marginal zone lymphoma, mantle cell lymphoma, and Waldenström macroglobulinemia—as well as chronic lymphocytic leukemia (CLL), including CLL that harbors a 17p deletion.
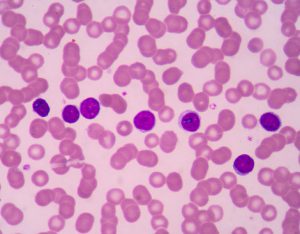
B cells. Marginal zone lymphoma arises in B cells in a part of lymph tissue called the marginal zone.
Marginal zone lymphoma, like mantle cell lymphoma, Waldenström macroglobulinemia, and most cases of CLL, arises in immune cells called B cells. The rationale for testing ibrutinib as a potential treatment for these types of cancer stems from the fact that ibrutinib targets the protein Bruton agammaglobulinemia tyrosine kinase (BTK), which is a component of a signaling pathway that promotes the survival and expansion of normal and malignant B cells.
The approval of ibrutinib to treat marginal zone lymphoma was based on results from the PCYC-1121 phase II clinical trial, which were presented at a scientific meeting in December 2016. In brief, they show that 46 percent of patients treated with ibrutinib had significant tumor shrinkage, with 3.2 percent having a complete response and 42.9 percent having a partial response. At the time the data were presented, the median duration of response had not been reached.
Given that the approval centered on response data, rather than overall survival, the companies jointly developing ibrutinib, Janssen Biotech Inc. and Pharmacyclics LLC, are required by the FDA to conduct a study to confirm that the drug improves survival for patients.
This approval “represents a welcome new oral option for the [marginal zone lymphoma] community,” said Ariela Noy, MD, hematologic oncologist at Memorial Sloan Kettering Cancer Center in New York and lead investigator of the study, in a news release.