FDA Approves First Use for an Anticancer Therapeutic Based on Tumor Biomarker, Not Tumor Origin
Tuesday marked a milestone for the oncology community: The U.S. Food and Drug Administration (FDA) announced its first approval of an anticancer therapeutic for use based on whether a patient has a tumor with certain biomarkers and not where in the body the tumor originated.
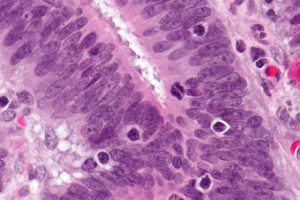
Microsatellite instability–high colorectal cancer is often found to have tumor-infiltrating immune cells. Image via Wikimedia.
The anticancer therapeutic in question is pembrolizumab (Keytruda), which works by releasing a brake called PD-1 on cancer-fighting immune cells called T cells. It is a member of a class of immunotherapeutics called immune checkpoint inhibitors.
The past few years have seen the FDA rapidly expand the number of approved uses for pembrolizumab and other immune checkpoint inhibitors. Until yesterday, each approval was for use in the treatment of a specific type of cancer, as defined by the location in the body where the tumor originated: melanoma, Hodgkin lymphoma, bladder cancer, head and neck cancer, and lung cancer in the case of pembrolizumab.
On Tuesday, the FDA approved pembrolizumab for treating certain adults and children who have unresectable or metastatic solid tumors found to be microsatellite instability–high or mismatch repair–deficient, including microsatellite instability–high or mismatch repair–deficient colorectal cancer. Specifically, it is approved for those patients whose tumors have progressed despite prior treatment and who have no satisfactory alternative treatment options.
What Makes Microsatellite Instability–High or Mismatch Repair–Deficiency a Good Biomarker for Pembrolizumab Treatment?
Maintaining DNA integrity is essential for a cell to remain healthy. The integrity of DNA is constantly under threat from errors that arise during cell multiplication or because of exposure to certain toxins and ultraviolet radiation from the sun. If DNA is not appropriately repaired, mutations accumulate, increasing the chance that a cell will become cancerous. Thus, cells have several interrelated pathways that they use to repair damaged DNA.
Mutations in genes encoding proteins involved in one of these pathways, the DNA mismatch repair pathway, can result in cells acquiring the microsatellite instability–high characteristic. Mismatch repair–deficiency and microsatellite instability are found in both hereditary and sporadic cancers arising at several anatomic locations, including the colon, endometrium, stomach, and rectum. In the case of colorectal cancer, it is estimated that about 15 percent of all cases diagnosed in the United States are microsatellite instability–high because of a DNA mismatch repair–deficiency. A significant proportion of these cases occur in individuals with Lynch syndrome, an inherited disorder caused by inherited mutations in DNA mismatch repair pathway genes that significantly increases a person’s risk of developing certain types of cancer, in particular colorectal cancer.
Numerous lines of research have led to the idea that cancers with a high mutational burden are more likely to be responsive to immune checkpoint inhibitors. Given that cancers with a mismatch repair–deficiency have a high mutational load, researchers set out to test in a clinical trial whether mismatch repair–deficient tumors were more responsive than mismatch repair–proficient tumors to pembrolizumab.
Results from this small study, which were published in The New England Journal of Medicine in 2015, suggested that this was indeed the case. Pembrolizumab treatment resulted in tumor shrinkage for 40 percent of the 10 patients with mismatch repair–deficient colorectal cancer, compared with none of the 18 patients with mismatch repair–proficient colorectal cancers. In addition, five of seven patients with mismatch repair–deficient cancers other than colorectal cancer responded to pembrolizumab treatment.
These data led the FDA to grant breakthrough therapy designation to pembrolizumab for the treatment of patients with microsatellite instability–high colorectal cancer in November 2015. This designation is designed to expedite the regulatory assessment of new therapeutics.
According to the FDA, the approval of pembrolizumab for unresectable or metastatic solid tumors found to be microsatellite instability–high or mismatch repair–deficient was based on data from 149 patients with microsatellite instability–high or mismatch repair–deficient cancers enrolled in five small clinical trials. Among these patients, 90 had colorectal cancer and 59 patients had one of 14 other types of cancer, including endometrial cancer, gastric or gastroesophageal junction cancer, pancreatic cancer, and biliary cancer.
Pembrolizumab treatment led to tumor shrinkage in 39.6 percent of the patients, with 11 patients having a complete response and 48 a partial response. The percentage of patients who had tumor shrinkage was similar among those with colorectal cancer and those with a different type of cancer: It was 36 percent among the patients with colorectal cancer and 46 percent among the patients with the other 14 types of cancer.
What is Next for Pembrolizumab?
The approval of pembrolizumab for unresectable or metastatic solid tumors found to be microsatellite instability–high or mismatch repair–deficient was based on response data, rather than overall survival data. Thus, the FDA requires Merck, the manufacturer of pembrolizumab, to conduct additional studies to confirm that the immune checkpoint inhibitor improves survival.
Given that recent data from early-stage clinical trials show that pembrolizumab may benefit some patients with gastric cancer and Merck announced on Tuesday that the FDA would make a decision on this potential use of pembrolizumab by Sept. 22, 2017, it is likely that the number of patients with cancer for whom pembrolizumab is a potential treatment option will continue to rise in the near future.



