FDA Approves New Treatment Option for Breast Cancer
Last week, the U.S. Food and Drug Administration (FDA) provided some good news for the breast cancer community just days before the start of Breast Cancer Awareness Month when it added a new molecularly targeted therapeutic to the armamentarium for oncologists treating patients with breast cancer: abemaciclib (Verzenio).
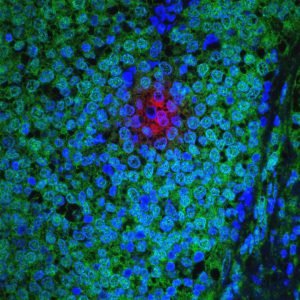
As discussed in a previous post on this blog, approximately three in every four breast cancers diagnosed in the United States are hormone receptor (HR)–positive. The discovery that the growth of these tumors is fueled by the hormones estrogen and/or progesterone led to the development of therapeutics that work in a range of ways to counter the effects of the hormones (endocrine therapy).
Unfortunately, some patients treated with endocrine therapy eventually have disease recurrence because their cancers become resistant to the therapy. Abemaciclib is now a treatment option for these patients because its approval is for the treatment of patients with HR-positive, HER2-negative, advanced or metastatic breast cancer that has progressed despite endocrine therapy. The molecularly targeted therapeutic can be used in combination with an endocrine therapy called fulvestrant or on its own, depending on the types of treatment a patient has already received.
Abemaciclib works by blocking the function of two proteins called cyclin-dependent kinase 4 (CDK4) and CDK6. These proteins play a role in driving cell multiplication, which is key for tumor growth.
The approval of abemaciclib in combination with fulvestrant was based on results from the MONARCH 2 phase III clinical trial. The results, which were published recently in The Journal of Clinical Oncology, showed that adding abemaciclib to fulvestrant improved progression-free survival for patients who had not received chemotherapy after their HR-positive, HER2-negative breast cancer had progressed during or following endocrine therapy. The median progression-free survival was 16.4 months among those who received abemaciclib and fulvestrant, compared with 9.3 months among those who received fulvestrant and placebo.
The approval of abemaciclib as a stand-alone treatment was based on results from the phase II MONARCH 1 clinical trial that were published recently in the AACR’s journal Clinical Cancer Research. In this study, abemaciclib was tested as a treatment for patients who had metastatic HR-positive, HER2-negative breast cancer that had progressed during or following endocrine therapy and whose metastatic disease had been treated with at least one cytotoxic chemotherapeutic. In brief, the data showed that 19.7 percent of the 132 patients who received abemaciclib as part of the trial had complete or partial tumor shrinkage.
Abemaciclib is the third CDK4/6 inhibitor to be approved by the FDA for treating certain patients with advanced or metastatic HR-positive, HER2-negative breast cancer. Palbociclib (Ibrance) was the first to be approved in February 2015 and ribociclib (Kisqali) the second, in March 2017.
The most common adverse effect reported in the abemaciclib clinical trials was diarrhea, whereas it was neutropenia in the palbociclib and ribociclib clinical trials. However, the percentage of patients who discontinued treatment as result of adverse effects was similar in all the clinical trials.
The emergence of a new class of therapeutics for treating endocrine therapy–resistant advanced or metastatic HR-positive, HER2-negative breast cancer illustrates how the armamentarium for treating previously recalcitrant diseases can strengthen rapidly. With our knowledge of cancer biology growing day by day, we hope that the number of treatment options for patients with other types of advanced cancer will soon expand too.