AACR Annual Meeting 2019: Global Burden of Pathogen-related Cancers
Persistent infections from pathogens are a major cause of cancer incidence worldwide. An analysis from 2012 indicates that more than 15 percent of new cancer cases were attributed to carcinogenic infection, and the top cancer-causing pathogens include H. pylori, human papillomavirus (HPV), hepatitis B virus (HBV), hepatitis C virus (HCV), and Epstein-Barr virus (EBV). Infections from some of these pathogens, especially HBV and HPV, can be prevented with approved vaccines.
The fourth plenary session of the AACR Annual Meeting 2019, titled “Pathogen-Related Cancers: Implications for Populations and Public Health,” was chaired by Acting Director of the National Cancer Institute, Douglas Lowy, MD, who helped to develop HPV vaccines. “There’s a substantial difference in the incidence of infectious agents involved with cancer in the less-developed world compared to the more-developed world,” said Lowy. He explained that about one out of four cancer diagnoses are attributable to infectious agents in less developed regions, compared with one out of eight in more developed areas. The talks in this session focused on the progress and challenges surrounding four key cancer-related pathogens.
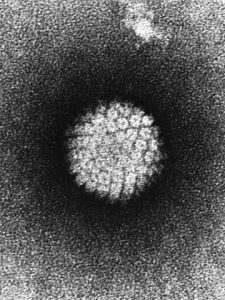
Therapeutic HPV vaccines for cervical cancer
Lowy introduced the first speaker of the session, Cornelia Trimble, MD, professor of gynecology and obstetrics at Johns Hopkins Medicine. Trimble gave the opening talk, titled “Therapeutic vaccination: lessons learned from HPV.”
Infection with HPV is estimated to cause more than 90 percent of anal and cervical cancers as well as a variety of other malignancies. HPV is a collection of over 200 related viruses; HPV types 16 and 18 cause the majority of cervical cancer cases. Vaccinations were designed to prevent infection from these two types, in addition to other strains of the virus.
In spite of vaccination efforts, cervical intraepithelial neoplasia (CIN), the precancerous condition of abnormal cellular growth on the surface of the cervix, remains common. CIN1 represents mild dysplasia, and CIN2/3 represents moderate to severe dysplasia.
Trimble noted that methods for intervention are under investigation, including the utilization of therapeutic vaccines against the HPV oncoproteins E6 and E7 as they are thought to be the essential drivers of HPV-associated cancers.
Trimble spoke of a vaccination strategy that targeted HPV16 E6/E7 antigens tested in women with CIN2/3; in addition to two HPV16 E7 DNA priming vaccines, patients received a boost vaccine containing a recombinant vaccinia virus that expressed HPV16 and HPV18 E6/E7. Compared to tissue samples taken before vaccination, post-vaccination samples showed increased immune responses, as indicated by increased lesional infiltration of CD8+ T cells in the stromal and epithelial compartments, as well as other factors. However, T-cell responses as measured in the blood were only modest, suggesting that conventional endpoints may not accurately reflect immune responses, Trimble noted.
She identified validating prognostic signatures of immune response in the blood and urine as important next steps.
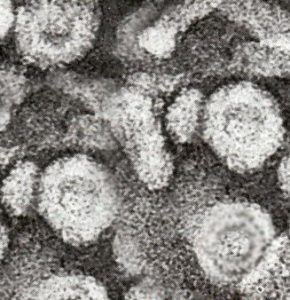
Early detection of nasopharyngeal cancer through circulating EBV DNA
Lowy next introduced Dennis Lo, MD, PhD, director of the Li Ka Shing Institute of Health Sciences and the Li Ka Shing professor of medicine and chemical pathology of The Chinese University of Hong Kong. Lo discussed “Screening for nasopharyngeal carcinoma using plasma Epstein-Barr virus DNA: Technology and clinical insights.”
Infection with EBV, a member of the herpes family, is extremely common; over 90 percent of the global population is infected. Most infections occur during childhood and often do not cause symptoms; teens or adults that become infected can develop mononucleosis. Following infection, the latent virus remains in the body, but is usually asymptomatic. However, EBV infection can increase the risk of nasopharyngeal cancer (NPC), which is especially prevalent in Southern China, noted Lo.
In Hong Kong, over 76 percent of NPC cases are diagnosed when the cancer has progressed to stage 3 or 4, Lo explained. Therefore, he is interested in quantifying circulating EBV DNA as a method for early NPC detection. Despite the widespread prevalence of EBV infection, Lo has previously shown that cell-free EBV DNA could be detected in 96 percent of patients with NPC compared to just 7 percent of healthy controls using real-time quantitative PCR.
Lo conducted a large-scale, prospective screening study focused on men aged 40-60 years aimed at detecting NPC through circulating EBV DNA measurements. Patients who tested positive for plasma EBV DNA received a nasal endoscopy and MRI assessment, and all participants had yearly follow-up assessments. Of the 20,174 participants, the researchers identified 34 cases of NPC, but the test did not have a high positive predictive value (PPV).
To enhance the utility of the test, Lo and colleagues utilized target-capture sequencing to measure the concentration and the fragment size of the circulating EBV DNA. They found that higher concentrations and larger fragments of EBV DNA correlated with NPC cases. By combining these two metrics, the researchers could better distinguish patients with NPC from subjects with persistently positive EBV DNA who did not have NPC. This method improved the PPV and reduced blood sampling to a single time point, Lo noted.
Targeting HBV and HCV for the prevention and treatment of hepatocellular carcinoma
Lowy introduced Jean-Michel Pawlotsky, MD, PhD, director of the Department of Molecular Virology and Immunology at Institut Mondor de Recherche Biomédicale (IMRB), to deliver his talk, “Hepatitis B and C virus-related hepatocellular carcinoma in the era of highly active antiviral therapies.”
Cases of liver cancer are increasing worldwide. From 1990 to 2015, liver cancer incidence increased by 75 percent, according to a recent analysis. Globally, deaths from liver cancer are attributed to HBV infection (33 percent), alcohol (30 percent), HCV infection (21 percent), or other factors (16 percent).
Pawlotsky first focused on the prevalence of HCV and how treating this virus can impact hepatocellular carcinoma (HCC). He noted that despite the success with the antiviral drug combinations that target various stages of the lifecycle of HCV, which yield cure rates of nearly 100 percent, the worldwide prevalence of HCV infection is estimated to be 71 million. While antiviral treatment has reduced HCC incidence and mortality, those with extensive fibrosis or cirrhosis still have an increased risk of the disease and should be more closely monitored.
Next, Pawlotsky talked about HBV prevalence and how treatment of the viral infection affects HCC. He explained that HBV infection affects an even larger percentage of the global population, with more than 250 million infected individuals. HBV vaccination significantly reduces HCC incidence, even if the vaccine is administered past childhood (ages 20-26). Once a person is infected with HBV, lifetime administration of antivirals can suppress viral replication and reduce HCC incidence, yet the infection itself remains incurable. The development of antiviral drugs that target alternative stages of the lifecycle of HBV are underway, Pawlotsky noted. Those chronically infected with HBV have a higher risk for HCC and should be more closely monitored, he added.
To conclude his talk, Pawlotsky spoke about the World Health Organization (WHO) goal to eliminate viral hepatitis as a major public health threat by 2030.
Advances and challenges for HIV-positive cancer patients
Lowy introduced the final speaker of the session, Ariela Noy, MD, medical oncologist at Memorial Sloan Kettering Cancer Center, who spoke about “HIV and malignancies: from despair to gene therapy.”
Infection with human immunodeficiency virus (HIV) increases the risk for several types of cancer, notably Kaposi sarcoma, anal cancer, and non-Hodgkin lymphoma. Because the virus attacks the immune system, those infected with HIV are more likely to become infected with other viruses.
Treatment of HIV-positive individuals with highly active antiretroviral therapy (HAART) has substantially lowered deaths associated with infection. These types of drugs work by lowering the viral load, decreasing the severity of the infection, and reducing the risk of HIV transmission. While HIV-positive patients treated with HAART have improved survival, this population has an increased risk for both AIDS-defining and non-AIDS-defining cancers, Noy explained.
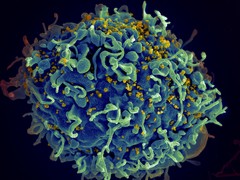
Noy discussed research advancements and clinical trial results for a variety of AIDS-defining cancers, including HIV-associated Burkitt lymphoma and diffuse large B-cell lymphoma. In the realm of non-AIDS-defining cancers, Noy talked about the challenges of lung cancer prevention in HIV-positive patients. While smoking prevalence in the average population is around 30 percent, in HIV-positive patients it is around 70 percent, she noted. Additionally, Noy mentioned early data suggesting that HIV-positive patients are more likely to be diagnosed with lung cancer at a young age, and the underlying mechanism for this finding remains unknown.
Noy concluded her talk by speaking about the exclusion of HIV patients in cancer clinical trials. She noted that while non-HIV patients who may have received many prior lines of therapy and likely have low CD4 counts are often included in clinical trials as their CD4 counts are not evaluated, HIV patients with acceptable CD4 counts are quite often denied inclusion in a trial because of their infection status. Noy, as part of an HIV Working Group, published recommendations for the enrollment of HIV patients in cancer clinical trials. Noy highlighted the final recommendation that “criteria should not be more stringent than for HIV-uninfected patients with the same disease or treatment history.”
Looking forward
Lowy concluded the session by highlighting the importance of identifying biomarkers for cancer-associated viral infections, and interventions, as these advances can help decrease the likelihood of developing cancer and increase survival. “There are lots of potential advancements and challenges that lie ahead, but I think that this morning really has exemplified what you can do if you identify an infectious agent as a cause of cancer,” Lowy said.