AACR Virtual Annual Meeting I: Results on a Targeted Therapeutic for Lung Cancer Support FDA Approval
Over the course of the two-day AACR Virtual Annual Meeting I, more than 61,000 people from 140 countries around the world registered to hear presentations about cutting-edge research that is driving progress against the collection of diseases we call cancer.
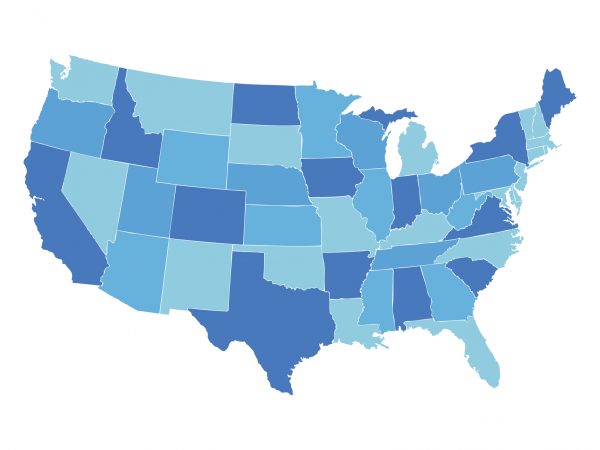
Lung cancer remains the leading cause of death from cancer in the United States, with more than 135,000 U.S. men and women expected to die from the disease in 2020 alone. This grim statistic hides, however, the good news that the U.S. lung cancer death rate has been decreasing slowly but steadily in the United States for the past 25 years.
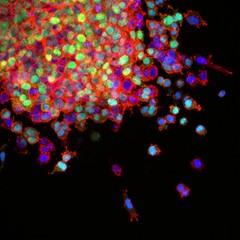
Part of the progress against lung cancer is being fueled by advances in treatment, in particular the rapid expansion in the number of molecularly targeted therapeutics developed as a result of genomics research identifying drivers of lung cancer. Data presented during the Lung Cancer Targeted Therapy Clinical Plenary Session of the AACR Virtual Annual Meeting I provided the basis for the U.S. Food and Drug Administration (FDA) approval of a new molecularly targeted therapeutic called capmatinib (Tabrecta) for treating certain patients with non–small cell lung cancer (NSCLC), highlighting how the AACR Annual Meeting has become a showcase for innovative experimental therapeutics that go on to benefit patients.
Edward B. Garon, MD, director of the Thoracic Oncology Program at the David Geffen School of Medicine at UCLA, opened his presentation about capmatinib by explaining that genomics research has shown that between 3 percent and 4 percent of NSCLCs harbor mutations in the gene MET that result in skipping of exon 14. These mutations are considered oncogenic drivers of lung cancer. “Patients with tumors that harbor these mutations have been reported to have poor outcomes with both cytotoxic chemotherapy and immunotherapy,” he noted.

Capmatinib targets MET, and Garon reported results from the GEOMETRY mono-1 phase II clinical trial, which was designed to evaluate capmatinib as a monotherapy for patients with stage IIIB or stage IV NSCLC that harbors MET gene alterations. The trial has seven different cohorts of patients. Garon reported results for cohorts 4 and 5b, both of which included patients who had NSCLC with MET exon 14 skipping mutations. The patients in cohort 4 had received at least one prior treatment for advanced NSCLC. The patients in cohort 5b had received no prior treatment for advanced NSCLC.
Among the 69 patients in cohort 4, the objective response rate was 40.6 percent. All of the responses were partial responses. Among the 28 patients in cohort 5b, the objective response rate was 67.9 percent, with one patient having a complete response and the other 18 having a partial response. The median duration of response was 9.72 months for those patients in cohort 4 and 11.14 months for those in cohort 5b.
Garon went on to discuss the responses of those patients who had brain metastases at time of enrollment in the trial. Research has shown that brain metastases occur in about 25 percent of patients with lung cancer and that these patients have a particularly poor prognosis. Among 13 patients who had brain metastases at time of enrollment in the trial, four patients had complete resolution of all the lesions in their brain and three had a partial response. Garon highlighted the case of a 73-year-old woman who had multiple brain metastases that had not been controlled by either whole brain radiation or treatment with the immunotherapeutic pembrolizumab (Keytruda). “All brain lesions had completely resolved by 12 weeks from the start of therapy [with capmatinib],” he said, noting that the patient continues to do well two years after starting capmatinib.
Grade 3 or greater adverse events were seen in only about a third of patients, noted Garon, who concluded that capmatinib had a manageable safety profile.
The FDA cited the data Garon presented as they decided to approve capmatinib for treating adult patients with metastatic NSCLC whose tumors have MET exon 14 skipping mutations, as detected by a companion diagnostic test called the FoundationOne CDx assay, which was approved by the FDA at the same time as capmatinib.
The approval of the molecularly targeted therapeutic capmatinib is an example of the progress being made in the treatment of lung cancer. However, as noted by Taofeek Owonikoko, MD, PhD, from Emory University School of Medicine in Atlanta, who was the discussant of Garon’s presentation, the duration of response to capmatinib was less than a year. He explained that this means we need more basic and translational research studies to clearly define the mechanisms of resistance to capmatinib and thereby inform combination treatment strategies.