AACR Virtual Annual Meeting II: Clinical Trials Plenary Session Highlights Immunotherapeutic Combinations and a Liquid Biopsy-based Strategy for Predicting Progression-free Survival
The second day of the AACR Virtual Annual Meeting II began with a clinical trials plenary session. Two of the session’s presentations, which focused on immunotherapy clinical trials, discussed the use of a therapeutic cancer vaccine and the inhibition of a new immune checkpoint protein as part of combination treatments. The third presentation aimed to determine if longitudinal liquid biopsies could help predict progression-free survival in a trial evaluating a targeted therapy for lung cancer.
Combining a personalized cancer vaccine with immune checkpoint blockade
The first talk in this session, delivered by Juanita Lopez, MB BChir, PhD, a consultant medical oncologist at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research in London, discussed results from a phase Ib clinical trial that evaluated the personalized cancer vaccine RO7198457 in combination with the PD-L1 inhibitor atezolizumab (Tecentriq) in patients with advanced solid tumors.

Therapeutic cancer vaccines rely on the identification and packaging of tumor-specific neoantigens that will activate the immune system to recognize and attack a tumor. Because most neoantigens are not shared between patients, a targeted neoantigen-specific therapy requires an individualized approach, said Lopez. As such, RO7198457 is made on a per-patient basis. To do this, Lopez explained, somatic mutations in the patient’s tumor are identified by next-generation sequencing (NGS), the immunogenic neoantigens are predicted, and then up to 20 selected neoantigens are encoded into messenger RNA (mRNA) molecules.
Due to its lipoplex nanoparticle formulation, RO7198457 is preferentially delivered to antigen-presenting cells (APCs), including dendritic cells in the spleen, Lopez said. The mRNA-based vaccine encodes the neoantigens, which are then expressed, processed, and displayed on these APCs. Further, the vaccine activates dendritic cells by binding to Toll-like receptors (TLRs) 7 and 8, resulting in the production of pro-inflammatory cytokines and the upregulation of co-stimulatory molecules, which stimulates the innate immune response. Both CD4 and CD8 T cells are activated by the vaccine, Lopez noted.
At the time of data cutoff, this trial had enrolled 30 patients in the dose escalation phase and 114 patients in indication-specific expansion cohorts. All patients received a combination of RO7198457 plus atezolizumab. In both cohorts, all patients had received prior treatment, and the majority of patients’ tumors had no or low expression of PD-L1.
While no dose-limiting toxicities were observed in either cohort, there were six adverse events that led to dose reduction of RO7198457. Treatment-related adverse events were primarily systemic reactions, which manifested as low-grade cytokine release syndrome, influenza-like illness, or an infusion-related reaction. However, all of these symptoms were transient, reversible, and manageable, Lopez noted.
Lopez showed response data for 28 patients in the dose escalation cohort. The combination had modest activity, as one patient with colorectal cancer had a complete response and one patient with triple negative breast cancer (TNBC) had a partial response. Lopez noted that the patient with TNBC was previously treated with immune checkpoint blockade and entered the study with visceral and lymph node metastases, which shrank or disappeared after the initial treatment. This patient remains well after 1.5 years on study.
Lopez then showed response data for 61 patients in the expansion phase who had not received prior immune checkpoint blockade treatment. She highlighted the objective response rate by tumor type, ranging from 4 percent in patients with TNBC to 30 percent in patients with melanoma. A randomized phase II study evaluating RO7198457 in combination with the anti-PD-1 antibody pembrolizumab (Keytruda) versus pembrolizumab alone in patients with previously untreated advanced melanoma has been initiated, Lopez noted.
The researchers also evaluated the peripheral blood of 63 patients to determine if treatment elicited neoantigen-specific T-cell responses. Over 70 percent of patients had detectable T-cell responses, with a median of 2.6 neoantigens per patient eliciting a response (ranging from one to nine neoantigens per patient). In the 14 patients where it was possible to delineate CD4 and CD8 T-cell responses, the researchers found that both types of T cells responded to the neoantigens.
Additionally, preliminary evidence suggested that RO7198457 stimulated T cells within the tumor microenvironment, as RO7198457-specific T-cell receptors (TCRs) were found in tumor tissue from a patient with rectal cancer. “A more dedicated analysis of intratumoral immune responses is now being evaluated in an ongoing, dedicated biomarker cohort,” Lopez said.
“In this trial, we show that we were able to generate tumor-specific immune responses in the majority of evaluable patients using a personalized cancer vaccine approach in combination with immune checkpoint blockade,” Lopez said in an AACR press release. “While the clinical response rate overall was low, this is likely because many of the patients treated in our study had very advanced disease, and were heavily pretreated,” she added.
Combining checkpoints: co-inhibition of TIGIT and PD-L1
While the immune checkpoint proteins CTLA-4, PD-1, and PD-L1 are common targets for inhibition in immunotherapy, another candidate has recently come to the fore: TIGIT, a receptor that is expressed on certain T cells and natural killer (NK) cells. TIGIT can inhibit the immune response by binding to its ligand, PVR, which is found on tumor cells and APCs. TIGIT can also block the activation of CD226, or DNAM-1, which is a positive regulator of the immune response.
Previous research has shown that TIGIT is co-expressed with PD-1, especially in tumor-infiltrating immune cells. This has prompted the hypothesis that inhibition of TIGIT may enhance the efficacy of PD-1/PD-L1 blockade. Indeed, preclinical research has shown that inhibition of TIGIT and PD-L1 decreases tumor growth and enhances survival synergistically in a murine model.
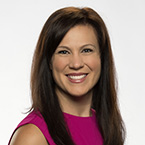
The second talk in this plenary session, delivered by Johanna Bendell, MD, from the Sarah Cannon Research Institute/Tennessee Oncology in Nashville, discussed the first-in-human phase I clinical trial of the anti-TIGIT antibody tiragolumab both as a single agent and in combination with atezolizumab in patients with advanced solid tumors.
The monotherapy arm, which evaluated tiragolumab alone, enrolled 24 patients, and the combination arm, which evaluated tiragolumab along with atezolizumab, enrolled 49 patients. Those with disease progression in the monotherapy cohort could cross over to the combination cohort; 12 patients (50 percent) crossed over to the combination arm. In both arms, around 40 percent of patients had received four or more prior cancer therapies.
No dose-limiting toxicities were observed in either arm. While 25 percent of patients treated with tiragolumab alone and 57 percent of patients treated with tiragolumab plus atezolizumab had a grade 3-5 adverse event, the majority of these adverse events were not considered related to study drugs.
In patients treated with tiragolumab alone, no objective responses were observed, although a subset of patients saw a reduction in their tumor size. In patients that received the combination therapy, partial responses were observed, particularly in patients with non-small cell lung cancer (NSCLC) whose tumors expressed PD-L1. No responses were observed in patients that crossed over from the monotherapy arm to the combination arm.
Based on pharmacodynamic data and clinical responses seen in the combination arm, the recommended phase 2 dose (RP2D) of tiragolumab was determined to be 600 mg every three weeks. Expansion cohorts were initiated to assess the combination of atezolizumab and tiragolumab (dosed at 400 or 600 mg) among patients who were immunotherapy-naïve and who had PD-L1-positive tumors.
Bendell showed data from an expansion cohort that included 13 patients with NSCLC. Among these patients, the overall response rate was 46 percent, which included two complete responses and four partial responses. Based on the safety and efficacy seen in this study, a randomized phase II clinical trial evaluating atezolizumab plus tiragolumab compared with atezolizumab plus placebo in patients with locally advanced or metastatic PD-L1-selected NSCLC as a first-line treatment was initiated. Initial results from this trial, recently presented at the American Society of Clinical Oncology (ASCO) annual meeting, indicated that the combination improved the overall response rate (31.3 percent versus 16.2 percent) and the median progression-free survival (5.4 months versus 3.6 months) compared with atezolizumab alone.
A phase III clinical trial comparing atezolizumab plus tiragolumab with atezolizumab plus placebo in patients with previously untreated, locally advanced unresectable or metastatic PD-L1-selected NSCLC has recently been initiated.
Combing through blood: using liquid biopsy to predict responses to a targeted treatment regimen
The final talk of this session was delivered by Ryan Hartmaier, PhD, associate director of Translational Medicine in Oncology Research and Development at AstraZeneca in Boston. His talk reviewed an exploratory biomarker analysis from the phase Ib TATTON study, which evaluated the MET inhibitor savolitinib in combination with the mutant-selective, third generation EGFR inhibitor osimeritinib (Tagrisso) in patients with EGFR-mutant NSCLC with MET amplification/overexpression whose disease had progressed on a prior EGFR inhibitor.
Previous research has indicated that the reduction or disappearance of EGFR mutations found in plasma—termed ctDNA clearance—has been associated with longer progression-free survival in patients with EGFR-mutant NSCLC treated with first-line osimeritinib. In this analysis of the TATTON study, Hatmaier and colleagues set out to determine if ctDNA clearance of EGFR-sensitizing mutations could be used to predict progression-free survival.

Hartmaier showed data derived from liquid biopsy samples collected eight and 12 weeks after treatment initiation. In this analysis, ctDNA clearance was defined as a detectable EGFR mutation at baseline that then became undetectable or dropped below 0.5 percent allele frequency in a longitudinal sample as assessed by the Resolution Bioscience ctDx Lung assay, he explained.
EGFR-mutant ctDNA was detectable at baseline in roughly 80 percent of evaluable patients. In one analysis, which included 34 patients treated with 600 mg of savolitinib, those with ctDNA clearance had a median progression-free survival of 9.1 months, while those without ctDNA clearance had a median progression-free survival of 3.9 months, corresponding to a statistically significant risk reduction of 66 percent.
“Our findings indicate that EGFR-mutant ctDNA clearance may be predictive of longer progression-free survival for patients with EGFR-mutant MET-amplified NSCLC with detectable ctDNA at baseline,” Hartmaier concluded.
Impactful clinical trials highlighted during AACR Virtual Annual Meeting I
Results from a host of clinical trials were presented in April during AACR Virtual Annual Meeting I, including practice-changing studies that led to two subsequent approvals from the U.S. Food and Drug Administration (FDA). Read our previous blog posts to learn about these approvals, which include a new targeted treatment for certain patients with NSCLC and an alternative dosing schedule for patients treated with pembrolizumab.