AACR Virtual Annual Meeting II: Guided by Genomics, A Global Effort to Treat Kids with Cancer
Pediatric cancer, while rare, is the leading cause of death by disease among children past infancy in the developed world. The World Health Organization notes that in most developed countries, more than 80 percent of children with cancer are cured, as opposed to only about 20 percent of those in many low- and middle-income countries.
Unlike adult cancers, pediatric cancers have low tumor mutational burden, making it challenging to find druggable targets and new treatment approaches. In the Presidential Select Symposium titled “Precision Pediatric Cancer Medicine – A Global Perspective,” moderator of the session and immediate Past President of the AACR, Elaine Mardis, PhD, FAACR, noted, “Three outstanding international speakers will present compelling evidence that multiplatform omics data can contribute significant evidence into the practice of pediatric oncology, providing more accurate subtyping, diagnosis, prognosis, and therapeutic indications for our youngest patients.”

Mardis went on to describe how large-scale efforts to study pediatric cancers provide evidence for the utility of therapeutics used in the treatment of adult cancers, such as small molecule inhibitors and antibody-based treatments, for pediatric cancers. This would also help limit the toxic and long-term side effects of traditional treatments with which most children with cancer are treated, in addition to improving their quality of life after cancer. Because the large-scale projects are designed to flow through the virtuous cycle of bench-to-bedside and back, they generate important hypotheses about the origins of pediatric cancers and refine our understanding of the disease, leading to the identification of new targets and therapies, Mardis added.
“Today, you will hear about pioneering countrywide efforts that knock down barriers to collaboration and networking for the benefit of all children with cancer, enabling data-, software-, and results-sharing with the goal to extend improvements in diagnosis, care, and outcome to all pediatric patients,” Mardis said.
The European Experience
As noted by the first presenter in the session, Stefan M. Pfister, MD, director of Preclinical Pediatric Oncology and division head of pediatric neuro-oncology at Hopp Children’s Cancer Center in Heidelberg, Germany, the cure rates for pediatric cancer have remained at around 80 percent for the last two decades, and adding more of the same type of treatments is unlikely to address the needs of the remaining 20 percent of the patients.

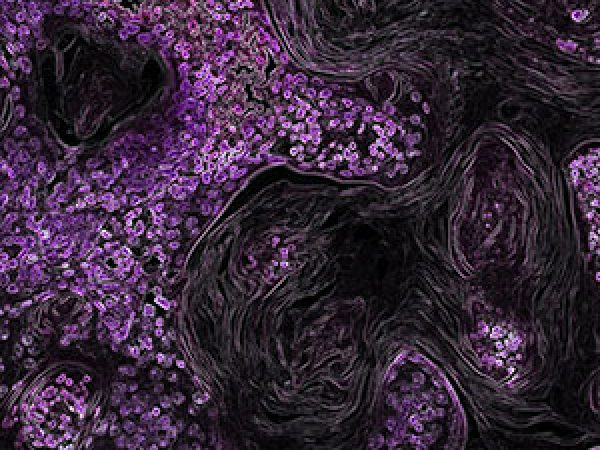
In his presentation, titled “A comprehensive European approach to precision pediatric cancer medicine,” Pfister elaborated on the efforts by the European precision pediatric oncology program called INFORM (short for Individualized Therapy For Relapsed Malignancies in Childhood), a multi-national registry spanning nine European countries, which offers comprehensive real-time molecular profiling for pediatric patients who have no standard treatment options. INFORM is complemented by corresponding programs in France, the Netherlands, the United Kingdom, and Denmark, Pfister noted. The group has enrolled more than 1,500 patients so far. Regular workflow includes whole-exome and whole-genome sequencing, RNA transcriptome sequencing, and DNA methylation analysis.
Speaking about detecting cancer predisposition alterations, Pfister said, “More than 90 percent of patients and families want to be informed about patient-relevant germline findings that we might detect in the tumors.” Through INFORM, the investigators have been successful in identifying potential drug targets, previously unidentified cancer predisposition markers, and potential biomarkers for many pediatric patients recruited to the program. About 5 to 10 percent of patients have had a tumor drug target identified, with appropriate treatment resulting in improved progression-free survival, according to Pfister.
The Australian Perspective
Michelle Haber, PhD, professor and executive director of Children’s Cancer Institute in Sydney, Australia, delivered a lecture titled “Zero Childhood Cancer: A comprehensive precision medicine platform for children with high-risk cancer in Australia.” Haber reviewed the goals and accomplishments of Zero Childhood Cancer, which was established in 2015 and aims to assess the feasibility of precision medicine in identifying targeted therapeutic agents for patients with high-risk pediatric malignancies. In this program, investigators perform comprehensive molecular profiling, including whole-genome sequencing of tumor and germline DNA, whole-transcriptome RNA sequencing, and methylation profiling of brain tumors and sarcomas. The results are utilized in conjunction with preclinical drug screening and testing, including patient-derived xenograft-based drug efficacy testing.

Following a successful pilot study with 50 children between 2016 and 2017, the investigators initiated a multicenter clinical trial in 2017, PRISM, with the goal of enrolling 400 children with high-risk or relapsed cancer across Australia by 2020. Through this approach, the investigators have been able to provide a recommended therapy for 31 percent of patients, and a reportable germline finding in 16.2 percent of patients. The germline predisposition rate was twice that of what was previously reported, Haber noted. The investigators have had a 21 percent success rate with drug efficacy testing so far. The current timeline from enrollment to a treatment recommendation report is eight weeks, Haber said. She added that 14 percent and 22 percent of the patients treated through this protocol have had complete response and partial responses, respectively.
The Zero Childhood Cancer program aims to expand the efforts to all children, adolescents, and young adults with cancer in Australia by 2023 to assess whether such a comprehensive program could change the model of cancer care differentially for children in different risk groups and improve health outcomes.
The Canadian Initiative
In a talk titled “PROFYLEing Cancer for KiCS: The Canadian Pediatric Precision Oncology Initiative,” David Malkin, MD, a clinician-scientist and pediatric oncologist in the Division of Hematology/Oncology, director of the Cancer Genetics program at SickKids, and senior scientist in the Genetics & Genome Biology Program at the SickKids Research Institute, talked about a large, Canadian interdisciplinary program, Precision Oncology for Young People, or PROFYLE, initiated in 2017.

The goal of PROFYLE is to transform the care of children, adolescents, and young adult cancer patients with hard-to-treat cancers in Canada through next-generation genomic approaches, including whole-genome and transcriptome sequencing. Samples from the patients are also used to develop models to identify new drug targets and therapies. The investigators have enrolled about 700 patients and have performed genome and transcriptome sequencing for about 500 of them so far. Data revealed that hypermutations are more common in pediatric cancers than previously thought. About 50 percent of the patients had at least one potentially actionable somatic variant. Overall, the investigators have been able to provide about 86 percent of clinicians a recommendation for further management of their patients, and 34 percent of the patients received a recommendation of change in treatment plan based on the evidence generated in this initiative.
Malkin briefly talked about PROFYLE 2.0, which has a focus on utilizing targeted therapies in clinical trials and will build further on the science behind the program, including expanding on experimental therapeutics and refining biomarkers of response and relapse.
New Award for Pediatric Cancer Research
Earlier in the conference, the AACR presented the first-ever AACR-St. Baldrick’s Foundation Award for Outstanding Achievement in Pediatric Cancer Research to St. Jude Children’s Research Hospital Chief Executive Officer James R. Downing, MD. Downing is also the director of the Molecular Pathology Laboratory at St. Jude Children’s Research Hospital and holds the Donald Pinkel Chair of Childhood Cancer Treatment.

Research on gene expression and pediatric cancer classification by Downing and his team led to the identification of unique gene expression profiles for subsets of acute lymphoblastic leukemia, a common type of pediatric cancer. Through the St. Jude-Washington University Pediatric Cancer Genome Project, Downing and colleagues sequenced the genomes of nearly 2,000 patients, leading to the identification of many genetic driver mutations previously not described in the onset and progression of pediatric cancer.