Patient Advocate Forum Explores the Effects of COVID-19
As the coronavirus pandemic took root in the United States, many hospitals and cancer centers temporarily suspended treatments and preventive screenings. Clinical trials of cancer drugs also paused, leaving some patients without access to potentially promising cancer treatments.
Now, with clinical trials for COVID-19 vaccines underway, cancer patients face a new dilemma as they feel left out of the discussion about how these vaccines might affect their cancer treatments and their overall health. Clinical trial participation during the pandemic became a central topic at the American Association for Cancer Research (AACR) Virtual Patient Advocate Forum on COVID-19 and Cancer, held last week. The forum brought together advocates from across the cancer community to provide the latest information on how COVID-19 is affecting patients with cancer.
To date, COVID-19 trials generally exclude participants who are on immunotherapeutic drugs, and some trials exclude people with any malignancy. Avrum Spira, MD, MSc, global head of the Lung Cancer Initiative at Johnson & Johnson Co., one of several companies that are testing COVID-19 vaccines in phase III clinical trials, said these exclusions will make it difficult to assess whether COVID-19 vaccines are safe and efficacious in patients with cancer.
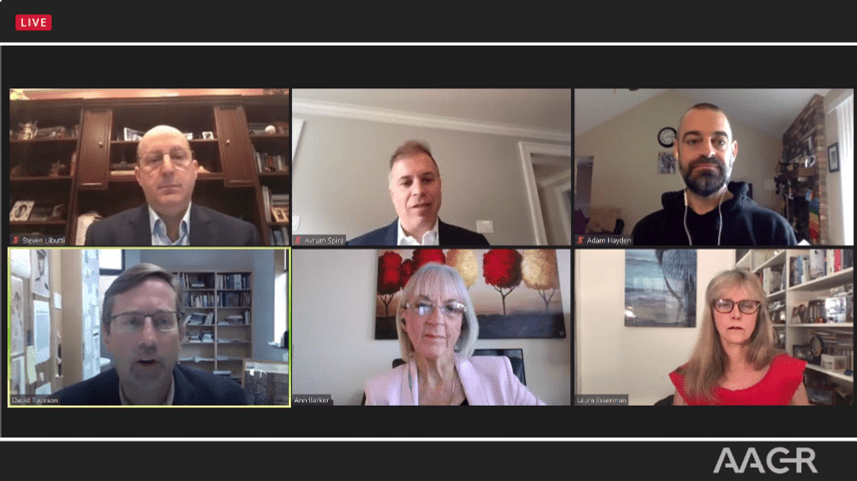
The panelists agreed that COVID-19 vaccines will be the best way for businesses and health care institutions to resume normal operations. But Anna D. Barker, PhD, Chief Strategy Officer of the Ellison Institute for Transformative Medicine at the University of Southern California and co-founder of the AACR’s Scientist↔Survivor Program (SSP), asked a poignant question: “How can cancer patients feel comfortable getting a COVID-19 vaccine if they haven’t been in the clinical trials?”
To that point, Laura Esserman, MD, MBA, director of the Carol Franc Buck Breast Care Center at the University of California San Francisco (UCSF), argued that many cancer patients could safely participate in clinical trials for COVID-19 vaccines, though trial criteria may need to be modified. Esserman, longtime principal investigator in the I-SPY breast cancer trial, said one reasonable modification would be to include cancer patients if they were two months or more past active treatment. She also noted that breast cancer patients who had been treated with hormone therapy should not be automatically excluded, since hormone therapy does not typically impact the immune system.
Spira agreed. “The patient advocacy community can raise your voices and remind industry that not all cancer patients are the same, and many of you could be included in clinical trials of a vaccine,” he said. “It’s still early on in these trials and your voices can make a difference.”
Meanwhile, Esserman believes clinical trials of cancer drugs should continue through the duration of the pandemic.
“This idea that we shut down the clinical trials in cancer is ridiculous,” she said. “Demand and insist that these trials stay open.”
Clinical trials are far from the only issue worrying patient advocates during the coronavirus pandemic. Adam Hayden, a writer and speaker who was diagnosed with glioblastoma in 2016, said cancellations and postponements of checkups and scans created severe anxiety in many cancer patients and survivors. Hayden, a past SSP participant, urged fellow patients and survivors to explore online sources of support, such as message boards and virtual support groups. Esserman agreed, noting that participation in one particular UCSF support group tripled when it began meeting online.
Some parting advice
Barker asked the panelists for one overarching recommendation for cancer patients and survivors as they continue to navigate their care during the pandemic. Here’s what they had to say:
David A. Tuveson, MD, PhD, FAACR and AACR President-Elect: “Stay socially connected to remain human and remain happy. Patients want to experience the touch and the sight of the physician. They can; we just have to be safe about it.”
Steven K. Libutti, MD, director of the Rutgers Cancer Institute of New Jersey: “Don’t sequester yourself to the point of not getting cancer care and not getting follow-up. Wear a mask and continue social distancing. We are going to get through this. But we have to be smart, we have to be safe, and we have to protect each other.”
Spira: “Vaccines are coming. That’s our way out; it will take a little longer, but they are coming. To cancer patients, demand that your voices be heard.”
Hayden: “We need a grassroots effort to make sure that cancer patients and survivors are included in clinical trials. But at the same time, the full burden of making this happen shouldn’t be placed on the patient population.”
Esserman: “Connection is key. Don’t be isolated. We may need to invest more in psychosocial support to ensure that we can maintain these connections.”
Barker: “There’s a silver lining to all of this. I have never seen in my entire life on the planet the kind of collaboration we have happening right now in science.”