January Editors’ Picks from AACR Journals
The new year has already ushered in some changes, but one thing stays the same. Each month, we’ll continue to feature the “must read” articles handpicked by the editors of the AACR journals. This month, the editors have chosen to highlight results from a clinical trial, a study on breast cancer chemoprevention, and an investigation of the role of nuclear pore complex formation in cancer, among other topics. And just in time for Cervical Cancer Awareness Month, two studies from this month’s picks examine prevention and development of cervical cancer. As always, studies featured here are freely available for a limited time.
Journal: Clinical Cancer Research (January 15 issue)
Hormone receptor (HR)-positive, HER2-negative breast cancer is the most common type of breast cancer diagnosed among premenopausal women; however, treatment options for premenopausal women remain limited. Approximately 40 percent of HR-positive, HER2-negative advanced breast cancers have mutations in phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA) that increase activity of the PI3K pathway. Therefore, inhibition of PI3K may be a potential therapeutic strategy. In this phase I clinical trial, the researchers evaluated the safety and efficacy of the PI3K inhibitors alpelisib or buparlisib in combination with the hormone therapies tamoxifen and goserelin in premenopausal women with HR-positive, HER2-negative advanced breast cancer. The recommended phase II doses were 350 mg for alpelisib and 100 mg for buparlisib. The most common treatment-emergent adverse events (TEAEs) were hypokalemia, hyperglycemia, and rash for patients in the alpelisib group and alanine aminotransferase increase, aspartate aminotransferase increase, and anxiety for the buparlisib group. Progression-free survival was 25.2 months for patients treated with the alpelisib regimen and 20.6 months for those treated with buparlisib. The authors conclude that alpelisib or buparlisib in combination with tamoxifen and goserelin is well tolerated and may be effective for premenopausal patients with HR-positive, HER2-negative breast cancer. This article was highlighted in the January issue, and a related commentary can be found here.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Roughly 90 percent of cervical cancers are caused by infection with the human papillomavirus (HPV), which spurred the development of HPV vaccines for the prevention of this disease. Routine vaccination was recommended in the United States in 2006. The quadrivalent HPV vaccine, which targets HPV types 6, 11, 16, and 18, was given until 2015, when the 9-valent HPV vaccine became available (which targets the same four HPV types as the quadrivalent vaccine, in addition to five additional types). However, the impact of HPV vaccination on invasive cervical cancers in the United States has yet to be fully elucidated, in part due to the long follow-up time required for such an analysis. In this study, the authors evaluated the incidence rates of invasive cervical cancer among women aged 15-29 years diagnosed during 1999-2017 using cancer registry data that covers nearly 98 percent of the U.S. population. They found that the incidence of both cervical squamous cell carcinoma (SCC) and adenocarcinoma (AC) decreased in this time frame. The largest decrease in SCC incidence was observed among women aged 15-20 years during 2010-2017, and the largest decrease in AC incidence was observed among women aged 15-20 years during 2006-2017. The authors note that women aged 15-20 are not typically screened for cervical cancer, and highlight the impact of HPV vaccination on invasive cervical cancer incidence in this population. This study was highlighted in the January issue and was featured in this recent blog post focused on cervical cancer awareness.
Journal: Cancer Prevention Research
Breast Cancer Chemoprevention: Use and Views of Australian Women and their Clinicians
Breast cancer chemoprevention is underutilized, despite its efficacy in reducing breast cancer risk. Here, the authors surveyed Australian women and their clinicians to identify the key factors hindering chemoprevention uptake. Survey respondents included 725 women whose lifetime risk of breast cancer was at least 1.5 times that of the general population and who were enrolled in the Kathleen Cuningham Foundation Consortium for Research into Familial Breast Cancer cohort study (kConFab). Respondents also included 221 clinicians. The survey showed that only 1.4 percent of kConFab women had taken chemoprevention. Furthermore, 52 percent of kConFab women, 3 percent of breast surgeons, and 35 percent of family physicians were unaware of its existence. Women reported side effects and inadequate information as the strongest barriers to chemoprevention, and reported long-term efficacy, wanting to stay healthy for their families, and abnormal breast biopsy as the strongest motivating factors for chemoprevention. Among breast surgeons, the strongest barrier to recommending chemoprevention was the side effects of medication; for family physicians, it was insufficient knowledge. For both clinician groups, the strongest facilitators were clear guidelines, strong family history of breast cancer, and better tools to select patients for chemoprevention. Based on these results, the authors suggest that targeting beliefs about side effects and enhancing clinician knowledge and resources could improve chemoprevention uptake. This article was featured in a spotlight in the January issue.
Journal: Clinical Cancer Research (January 1 issue)
The anti-EGFR monoclonal antibody cetuximab (Erbitux) is used for the treatment of metastatic colorectal cancer. While RAS mutation status can guide treatment selection, with RAS wild-type tumors showing the greatest benefit, the predictive utility of expanded mutations to the RAS and BRAF genes have yet to be evaluated among patients treated with cetuximab. In light of this, the authors conducted a retrospective analysis of the CO.17 trial which compared cetuximab with best supportive care among patients with metastatic colorectal cancer. Using the highly sensitive digital PCR method BEAMing (which stands for beads, emulsion, amplification, magnetics), the researchers evaluated microdissected tissue samples for mutations in the KRAS and NRAS genes (at codons 12/13/59/61/117/146) and for the V600E mutation in the BRAF gene. Data from samples that were not analyzed via BEAMing but rather via prior Sanger sequencing were also included. In patients with RAS/BRAF wild-type tumors, treatment with cetuximab resulted in improved overall survival (OS) and progression-free survival (PFS) compared with best supportive care. Conversely, treatment with cetuximab did not improve OS or PFS among patients with KRAS-, NRAS-, or BRAF-mutant tumors. Tests of interaction found that RAS, but not BRAF, mutations were predictive of cetuximab benefit. Among patients whose tumors were previously analyzed using Sanger sequencing and were categorized as KRAS wild-type, 14 percent had a mutation in KRAS codon 2 after analysis with BEAMing. The authors conclude that more sensitive assays for the detection of specific somatic mutations can improve patient selection for treatment with cetuximab. This article was highlighted in the January 1 issue.
Journal: Cancer Research (January 15 issue)
Functional Precision Medicine Identifies New Therapeutic Candidates for Medulloblastoma
Medulloblastoma, a type of central nervous system tumor that develops in the cerebellum, is one of the most common malignant pediatric brain tumors. While research indicates that these tumors are heterogenous and can be classified into four distinct subgroups [WNT, Sonic hedgehog (SHH), Group 3, and Group 4], most patients receive similar treatments for their cancer, and roughly a third of patients die from their disease. To better understand the molecular and cellular differences between the different subtypes of medulloblastoma, and to potentially uncover any therapeutic candidates for these subtypes, the study authors evaluated a panel of 20 medulloblastoma patient-derived xenografts (PDX). They used a variety of techniques, including DNA sequencing, gene expression profiling, and high-throughput drug sequencing, and discovered that while most medulloblastomas do not have actionable mutations, different subtypes were sensitive to specific drugs. Notably, Group 3 medulloblastomas, the most aggressive subtype of the disease, were sensitive to actinomycin D, a drug that is rarely used to treat medulloblastoma. The authors note that their approach is feasible in the clinical setting, and could provide new therapeutic options for patients with newly diagnosed or recurrent disease.
Journal: Cancer Discovery
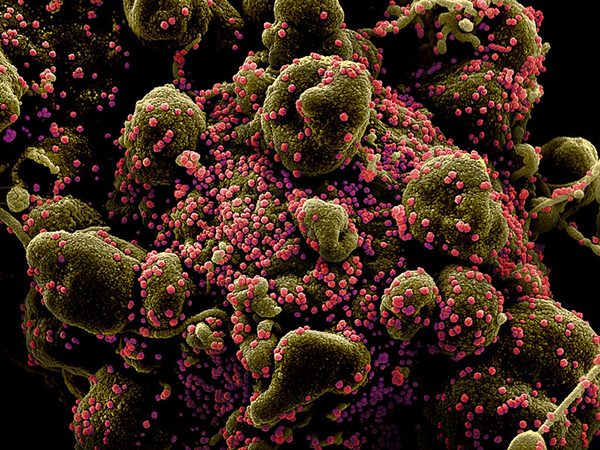
Inhibition of Nuclear Pore Complex Formation Selectively Induces Cancer Cell Death

Accumulating evidence suggests that cancer cells have higher numbers of nuclear pore complexes (NPCs) when compared to normal cells, but the impact of NPC number on cancer cell physiology and survival remains unclear. In this study, the authors observed that NPC formation is associated with cellular proliferation and is required for the survival of cancer cell lines. Depletion of essential nucleoporins inhibited NPC formation and led to cell death in cancer cells. In contrast, inhibition of NPC formation in normal cells did not induce cell death but led to a reversible cell cycle arrest instead. Consistent with this observation, the authors demonstrated that suppression of NPC formation affected several transformation-associated cellular processes and led to nuclear transport abnormalities, genetic alterations, and the accumulation of DNA damage. Reduction of NPC number led to tumor regression in melanoma and colorectal xenograft tumors. The authors propose NPC formation as a potential therapeutic target for cancer treatment. This article was highlighted and featured on the cover of the January issue.
Journal: Molecular Cancer Research
Progesterone Receptor is a Haploinsufficient Tumor Suppressor Gene in Cervical Cancer
According to the World Health Organization, cervical cancer is the fourth most common cancer among women globally, with an estimated 570,000 individuals receiving a cervical cancer diagnosis in 2018. While the female sex hormones estrogen and progesterone have been implicated in cervical cancer incidence, the specific roles of these hormones and their associated receptors in cervical carcinogenesis have yet to be fully elucidated. Using a human papillomavirus (HPV) transgenic mouse model, the study authors evaluated how deletion of the Pgr gene (which encodes for progesterone receptor) affected tumorigenesis. They found that deletion of one Pgr allele in the cervical epithelium promoted the spontaneous development of cervical cancer just as efficiently as deleting both Pgr alleles. The study authors also interrogated The Cancer Genome Atlas (TCGA) and found that PGR heterozygosity was common in human cervical cancer, and that low PGR expression was associated with a poor prognosis in young patients with the disease. The authors suggest that PGR is a haploinsufficient tumor suppressor gene in the uterine cervix that may be a promising therapeutic target for the treatment of cervical cancer. This article was highlighted in the January issue.
Journal: Molecular Cancer Therapeutics
Cancer cells are known to have altered metabolism compared with normal cells, with a significant subset of cancer cells relying on intracellular serine/glycine synthesis. While this pathway represents a potential therapeutic target, previously developed inhibitors of enzymes involved in serine/glycine synthesis did not reach clinical trials due to unfavorable pharmacokinetic profiles. With a focus on previously approved drugs, the study authors used a yeast model system that upregulates serine/glycine synthesis in response to stress to identify potential inhibitors of this metabolic pathway. Compounds were subsequently evaluated both in vitro and in vivo to investigate their antiproliferative effect on serine/glycine synthesis-addicted cancer cells. Following a variety of mechanistic analyses, the study authors found that the antidepressant sertraline (Zoloft) could disrupt serine/glycine synthesis through inhibition of serine hydroxymethyltransferase (SHMT). Further, the antiproliferative activity of sertraline was enhanced when combined with mitochondrial inhibitors in breast cancer mouse xenografts. The authors conclude that sertraline, which is already approved as an antidepressant and used extensively in the United States, may have applications for the treatment of serine/glycine synthesis-addicted cancers. This article was highlighted in the January issue.
Journal: Cancer Research (January 1 issue)

The angiopoietin-2 (ANGPT2) protein has diverse functions in cancer cells and has been explored as a potential therapeutic target. ANGPT2443 is a naturally occurring, alternatively spliced isoform that lacks the amino-terminal oligomerization domain and is expressed at increased levels in cancer cells. Here, the authors examined the impact of the ANGPT2443 isoform on cancer cell processes to determine functions of the amino-terminal oligomerization domain of full-length ANGPT2. They found that ectopic expression of Angpt2443 had diverse effects in various mouse models. In a mouse model of angiogenesis, for example, Angpt2443 expression impaired vein development; in mammary gland tumor models, its expression affected primary tumor growth and vascularization. In the presence of metastatic cells, Angpt2443 expression led to the destabilization of lung vasculature and led to lung metastasis. The authors concluded that the amino-terminal oligomerization domain of ANGPT2 contributes to vascular remodeling, mammary gland tumor growth, and lung metastasis. This article was featured on the cover of the January issue. A related commentary can be found here.
Journal: Cancer Immunology Research
The Prognostic Role of Macrophage Polarization in the Colorectal Cancer
Macrophages are one of the most common non-cancer cells in human tumors, including in colorectal tumors. However, studies examining how different tumor-associated macrophage populations affect outcomes have found contradicting results. In this study, the authors examined the association of macrophage polarization and density on the cancer-specific survival of 931 patients with colorectal cancer. They used multiplexed immunofluorescence and machine learning to visualize multiple markers of macrophage polarization and define M1-like and M2-like macrophages. After controlling for tumor stage and microsatellite instability status, they found that high tumor stromal density of M2-like macrophages was associated with worse cancer-specific survival. While higher tumor stromal density of M1-like macrophages was not prognostic, a high ratio of M1:M2 density was associated with better survival. In contrast, overall macrophage density was not associated with prognosis. Together, the results of this study suggest that macrophage polarization—and not overall macrophage density—is associated with cancer-specific survival in patients with colorectal cancer. This article was featured on the cover of the January issue.
Journal: Blood Cancer Discovery
Sphingosine-1-phosphate (S1P) is a bioactive sphingolipid that modulates proliferation, migration, and inflammation in various cell types. However, the role of S1P in normal hematopoiesis or in the development of stem cell malignancies, such as acute myeloid leukemia (AML), remains under investigation. S1P signals through S1PR1-5 receptors, and in the current study, the authors demonstrate that the expression of certain receptors were enriched in specific mature lineages. Focusing on the S1PR3 gene, the authors demonstrate that its expression was limited to monocytes and granulocytes, suggesting a role in myeloid fate specification. Overexpression of S1PR3 promoted myeloid differentiation in human hematopoietic stem and progenitor cells (HSPC) both in vitro and in vivo, and elevated expression of S1PR3 activated inflammatory programs in normal hematopoietic stem cells (HSC) and leukemic stem cells (LSC). Furthermore, S1PR3 expression was induced by inflammatory cytokines, which also promoted myeloid differentiation. In AML patient samples, S1PR3 expression could distinguish primitive AML from mature AML with different sensitivity to chemotherapy, indicating that S1PR3 could be used as a potential biomarker for these AML subsets. Finally, the authors report that S1PR3 expression was correlated with low LSC activity and that the S1P antagonist fingolimod (Gilenya) reduced LSC frequency and decreased leukemia burden in vivo, suggesting that modulation of S1PR3 could represent a potential therapeutic strategy to disrupt LSC function in AML. This article was highlighted and was featured on the cover of the January issue. A related commentary can be found here.