Artificial Intelligence for the Diagnosis and Treatment of Lymphoma
What if a machine could “think” like a doctor and diagnose and treat a disease? This is one of the long-term goals for the field of artificial intelligence (AI).
In a session co-sponsored by the American Association for Cancer Research (AACR) at the International Conference on Malignant Lymphoma, researchers provided an overview of AI and its potential applications in managing lymphoma, a group of blood cancers that begin in immune cells known as lymphocytes.
According to Luca Gambardella, PhD, the first presenter of the session, AI aims to solve problems using methods inspired by the way people innately think, sense, and learn. AI has gained interest in the past decade, with both academic and industry partners studying and investing in this technology.
AI applications currently under investigation include medical devices, wearable robotics, and machine learning (and the more automated version known as deep learning). Gambardella explained that AI could ultimately allow for the automatic adjustment of settings on medical devices, such as ventilators, according to the characteristics of each patient and the environment. He added that AI for wearable robotics, including prosthetics and wheelchairs, could improve a patient’s quality of life by automatically responding to environmental cues.
Machine learning and deep learning aim to use AI to extract knowledge from large datasets in order to accurately classify patients or cancers and/or predict outcomes. Additional presentations from the AACR-ICML Joint Session: Artificial Intelligence in Lymphoma Diagnosis and Treatment explored the use of machine and/or deep learning for the analysis of histopathology images, the identification of oncogenic driver events, and the improvement of clinical trials.
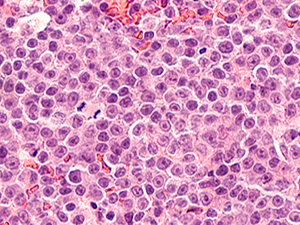
The diagnosis of lymphoma often involves examining histopathology images for cancer cells. As explained by Pierre Brousset, MD, PhD, manual analysis of histopathology images requires years of training, can be subjective, and is not fully reproducible, particularly for the analysis of rare cancers. Deep learning, on the other hand, has the potential to automatically recognize patterns in histology images with high accuracy and reproducibility, and has been employed in investigational settings to classify lung cancer subtypes, characterize tumor composition, predict prognosis, determine Gleason grade in prostate cancers, and identify clinically actionable mutations. However, challenges remain to this technology, including the variability in tissue staining between laboratories that can interfere with AI algorithms. Perhaps the biggest limitation, according to Brousset, is the stringent requirements for an appropriate training set, which must include a multitude of data and must be well annotated and representative of the target population.
In another presentation from the session, Dan Landau, MD, PhD, discussed the use of deep learning to identify oncogenic driver mutations from DNA methylation data. Aberrant DNA methylation is common in a variety of cancer types, including lymphomas. While DNA methylation changes are widespread throughout the genome, only a subset will lead to cancer development. Deep learning has the potential to help distinguish oncogenic driver methylation events from benign passenger events, but utilizing it has thus far been challenging. Landau described MethSig, an algorithm developed by his research team that factors in gene-specific methylation signatures, gene expression, replication timing, and background methylation rates to identify driver methylation events. In validation experiments, which included analyses of data from patients with chronic lymphocytic leukemia, Landau and colleagues found that MethSig identified driver methylation events with greater accuracy than previous methods, and that it could also predict patient outcomes. This research was recently published in Cancer Discovery, a journal of the AACR.
The final presentation of the session, delivered by Paul Trichelair, examined how deep learning could address some of the challenges associated with lymphoma clinical trials, including trial duration and reproducibility. Trichelair noted that clinical trials for diffuse large B-cell lymphoma, an aggressive type of non-Hodgkin lymphoma, require a median of 4.5 years to finish enrollment and a median of over eight years to publish results. In addition, efficacy results from phase II clinical trials often do not carry through to phase III trials. To reduce the time required for patient enrollment, Trichelair suggested using deep learning to identify prognostic biomarkers from histology images or PET scans that could be used for patient selection. He also proposed assessing long-term efficacy through surrogate endpoints, which could be detected earlier by using deep learning to analyze PET scans. To better predict efficacy in phase II trials, Trichelair suggested using external control arms instead of performing single-arm trials; this would allow researchers to compare the investigational treatment to the standard of care during early-phase clinical trials. He explained that deep learning could help account for the confounding variables associated with external control arms.
Together, the results from this session highlight some of the exciting applications for AI in cancer research, hinting at what Gambardella described as “a hybrid world where humans and AI [will] collaborate and cooperate.”
For additional information on AI in cancer research, be sure to check out this blog post on AI research presented at the AACR Virtual Annual Meeting, held last year. Upcoming meetings on blood cancer research include the AACR Virtual Meeting: Precision Medicine Strategies to Improve Therapy of Diffuse Large B-Cell Lymphoma (DLBCL) and the AACR Special Conference: Acute Myeloid Leukemia and Myelodysplastic Syndrome.



