Molecular Targets 2021: Getting CRISPR Where It Needs to Go
One year, to the day, after winning the Nobel Prize in Chemistry for her groundbreaking work on the genetic editing tool CRISPR, Jennifer A. Doudna, PhD, FAACR took the stage for the keynote address at the 2021 AACR-NCI-EORTC Virtual International Conference on Molecular Targets and Cancer Therapeutics. The buzz surrounding CRISPR has revolutionized fields from medicine to agriculture to bioethics since the adaptation of the system for gene editing in 2012, and Doudna’s keynote, titled, “CRISPR and gene modification for cancer therapeutics,” demonstrated that its potential is only beginning to be realized.
“Over the last almost-decade, it’s been extraordinary to see how fast this technology has been adopted and engineered to do different things,” said Doudna. “This system is readily altered, making it a truly programmable type of tool.”

Researchers around the world have used CRISPR and other gene editing techniques to edit plants in ways that address sustainability and hunger issues; to investigate the genetic and molecular mechanisms of disease; and, recently, to correct disease-causing mutations in human patients. Doudna told the story of the first person to receive CRISPR therapy in the United States, who was treated for sickle-cell anemia in 2019. The treatment used the patient’s own bone marrow, which was harvested, edited to correct the mutation, and returned to the patient’s body. Because the treatment edited the stem cells that produce red blood cells, the patient has not required additional infusions, Doudna said.
Since then, dozens more have been treated for various blood disorders, including thalassemias. However, safely targeting diseases of solid tissue, or diseases with more complicated genetic underpinnings, will require more creative approaches. The biggest challenge, Doudna explained, lies in the delivery of CRISPR enzymes to various tissues.
“Understanding how to deliver these molecules in situ, in patients, is going to open the door to many, many more exciting opportunities,” she said.
A viral shell for CRISPR enzymes
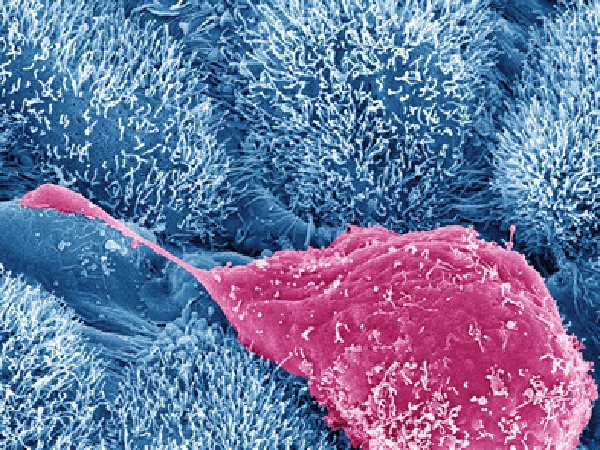
While CRISPR-based therapies that edit cells outside a patient’s body have showed promising results, there are limits to the ways such tools can be used. Cancer cells, for example, cannot be removed and reimplanted in this way. For this reason, Doudna explained, an important area of focus in the CRISPR field is the delivery of CRISPR enzymes to various parts of the body, including solid tissue.
One approach that Doudna and colleagues have taken is to package the CRISPR machinery inside of a virus-like envelope called a capsid. In this approach, the researchers can engineer cells in culture to transcribe all the genes necessary for CRISPR function, envelop the assembled complexes inside the capsid, and secrete the capsids for easy harvesting.
To accomplish this, the researchers transfect cells with genes encoding the Cas9 enzyme, the guide RNA that directs the enzyme to its target sequence, a DNA template to direct repair of the resulting double-stranded break, and the viral capsid. Inside the cell, the guide RNA forms a complex with the Cas9 enzyme, and tags on the enzyme and the DNA template direct them to be packaged into the capsid.
Using this system, researchers can also add genes for peptides, such as glycoproteins, to be expressed on the surface of the capsid to target the particles to various cell types, Doudna said.
The researchers can then harvest the virus from the cultured cells and use it to infect and edit their cells of interest. Thus far, they have only used this approach to edit immune cells external to a patient, but Doudna is optimistic that the system can eventually be injected directly into humans.
“A long-term goal of this work is to have the process be efficient enough that one could actually do this kind of editing in patients without requiring ex vivo editing,” she said.
Editing immune cells to fight solid tumors
Although safe and efficient delivery of CRISPR systems directly into patients will take some time, editing cells harvested from patients could still drive progress toward using CRISPR to help treat cancer.
Cell-based immunotherapies, such as chimeric antigen receptor (CAR-T) therapy, involve the genetic engineering of a patient’s T cells to target antigens presented on the surface of a tumor cell. Currently, T cells are harvested from a patient, virally infected with a chimeric antigen receptor, expanded in culture, and infused back into the patient. This therapy has proven effective for various blood cancers, but more genetic modifications would be needed to expand its efficacy to solid tumors. Subsequent genetic alterations would require extra steps, making the process less efficient.
The CRISPR encapsidation technique Doudna described, however, could present an all-in-one approach to knock in the gene for a chimeric antigen receptor and knock out genes—such as TRAC, TGFβ, or PD-1—that suppress T cell function or prevent infiltration of solid tumors. By packaging the elements for both alterations within the same capsid, the researchers can ensure efficient delivery of both complexes to the same cell.
Further, Doudna and colleagues have shown that they can target these capsids to specific cell types. In a co-culture system of different types of T cells, they were able to knock in a green fluorescent protein to CD4+ T cells without changing CD8+ T cells. Doudna believes that the ability to discriminate between different types of cells would reduce off-target effects if the immune-altering technology moves from the lab into the patient.
“Experiments are ongoing where we’re trying to do that kind of targeted editing in animals,” Doudna said. “It’s difficult to get to levels of editing that will be clinically meaningful. Nonetheless, it’s a very important thing to be working on, because figuring that out will open the door to so many opportunities.”
Looking to the future
Sparked by questions from the audience, Doudna speculated on various other ways CRISPR may improve cancer treatment. One possibility involved the use of CRISPR for cancer diagnostics.
Cas family RNA nucleases, such as Cas13, can be used to detect small amounts of an RNA message present in a biological sample. Such systems can be engineered to release a fluorescent probe upon cleaving the RNA target sequence, which allows for the rapid, low-cost detection of RNA transcripts.
Doudna and colleagues are working to develop a CRISPR-based assay for detection of SARS-CoV-2 based on this technology, which was the subject of a recent study in Nature Chemical Biology. When asked if this idea could be applied to the detection of cancer, Doudna was optimistic.
“Direct RNA detection that doesn’t require conversion to DNA or PCR amplification has some real advantages,” she said. “You could imagine doing the same kind of thing for cancer-specific transcripts, and I think that could be extraordinary.”
Doudna was also asked to speculate on whether her viral encapsidation system could be used for tumor types that aren’t easily accessible, such as the brain. Citing a recent paper in the New England Journal of Medicine, in which researchers targeted Cas9 and a CRISPR guide RNA to the liver using lipid nanoparticles, Doudna suggested that if existing technologies couldn’t take CRISPR to the brain, someone would find an approach that worked.
“The brain would be a major target—something that we’re very interested in,” she said. “It continues to be a challenge, but that lipid nanoparticle data shows that if you figure out the delivery, the editing itself can be highly effective and efficient.
“Looking at the pace at which the field has developed over the last decade is sort of mind-blowing,” Doudna continued. “I see things only accelerating from here. It’s not slowing down.”