AACR Journal Editors Share Selected Articles
As we finally welcome spring, enjoy this hand-picked selection of articles brought to you by the editors of the AACR journals. This month’s highlights include a study showing that improved cancer detection before metastasis could significantly reduce mortality rates, especially in populations with higher cancer burden; a report on the preclinical development of a novel histone deacetylase inhibitor for the treatment of solid tumors; and an article detailing the preparation of a beverage containing freeze-dried watercress to use in a chemoprevention clinical trial, among others. As always, these articles are freely available online for a limited time.
Journal: Cancer Research (March 15 issue)
Combined Inactivation of CTPS1 and ATR Is Synthetically Lethal to MYC-Overexpressing Cancer Cells

The Myc oncogene is frequently overexpressed in cancer cells, leading to increased protein synthesis and a high demand for ribosomal RNA. Two Myc target genes, CTPS1 and CTPS2, drive the production of cytosine nucleotides used to synthesize DNA and ribosomal RNA. In this study, the researchers investigated whether CTPS inhibition could induce DNA replication stress by limiting cytosine availability in Myc overexpressing cells. The researchers treated cells with the CTPS inhibitor 3-deazauridine (DAU), which reduced proliferation of Myc-overexpressing cells significantly more than cells with normal Myc levels. DAU treatment drove S-phase cell cycle arrest and induced several markers of DNA replication stress. The researchers knocked down CTPS1 and CTPS2 in Myc-overexpressing cells to further validate their findings and found that only CTPS1 knockdown inhibited proliferation and promoted replication stress. The researchers hypothesized that replication stress may sensitize cells to an inhibitor of the DNA checkpoint protein ATR. Cotreatment with DAU and an ATR inhibitor damaged DNA exclusively in Myc-overexpressing cell lines and drove apoptosis of the cells in culture and in a mouse model. The researchers suggest that combined inhibition of CTPS1 and ATR creates a synthetic lethality effect that could be used to treat patients with Myc-driven tumors. This study was featured on the cover of the March 15 issue, and a related commentary can be found here.
Journal: Clinical Cancer Research (March 15 issue)
Two subtypes of liposarcoma—well-differentiated and dedifferentiated liposarcomas—are often driven by genetic amplification of the p53 inhibitor MDM2 and the cell cycle gene CDK4. In prior studies, researchers treated liposarcoma patients with an MDM2 inhibitor plus the standard of care doxorubicin, but severe hematotoxicities prevented further exploration. In this phase Ib clinical trial, the researchers treated 74 patients with the MDM2 inhibitor siremadlin in combination with the CDK4/6 inhibitor ribociclib (Kisqali) to assess safety and determine the optimal dosing regimen. Patients were assigned to one of three dose regimens: daily siremadlin and ribociclib on days 1-14 of a four-week cycle (regimen A); siremadlin on day 1 plus ribociclib on days 1-14 of a three-week cycle (regimen B); or siremadlin on day 1 plus ribociclib on days 1-14 of a four-week cycle (regimen C). Patients treated with regimen A experienced a high rate of hematological toxicity, leading to the discontinuation of that treatment arm. Regimen B was selected as the recommended dose for expansion. Two of the 29 patients treated with regimen B experienced a partial response, and 17 of the 29 patients experienced stable disease. Treatment-related adverse events were observed in 100 percent of patients at this dose level, with 69 percent of patients experiencing an adverse event of grade 3 or 4. The authors suggest that this preliminary safety and efficacy profile warrants further clinical development of this combination therapy. This study was highlighted in the March 15 issue.
Journal: Molecular Cancer Research
Over 80 percent of colorectal cancers harbor activating mutations in the Wnt signaling pathway, and drugs targeting upstream regulators of Wnt signaling are in development. However, recent attempts to establish colorectal cancer subtypes have found that lower Wnt signaling activity correlates with poorer prognoses. In this study, the researchers overexpressed a dominant negative form of the Wnt transcriptional effector LEF1 in two colorectal cancer cell lines, thereby blocking Wnt-mediated transcription. Cells with decreased Wnt signaling were more migratory and, when injected into mouse colonic walls, showed more invasion and metastases than cells with unsuppressed Wnt signaling. The researchers created a second genetic model of Wnt signaling disruption by knocking out LRP6—a Wnt coreceptor—in colorectal cancer cells. The promigratory effects of LRP6 knockout took longer to manifest than those of dominant negative LEF1, and LRP6 knockout cells did not produce more metastases than control cells in a mouse model, although LRP6 knockout cell produced larger metastases than did control cells. This suggested that Wnt signaling suppression can have a “graded” effect based on where in the pathway signaling is disrupted. Gene expression analysis of mouse tumors formed from dominant negative LEF1-expressing cells revealed expression patterns characteristic of invasion and stemness, as well as downregulated inflammation in the surrounding stroma. The authors suggest that targeting β-catenin-mediated Wnt signaling in colorectal cancer could have unintended consequences of increasing invasion and metastasis. This study was highlighted in and featured on the cover of the March issue.
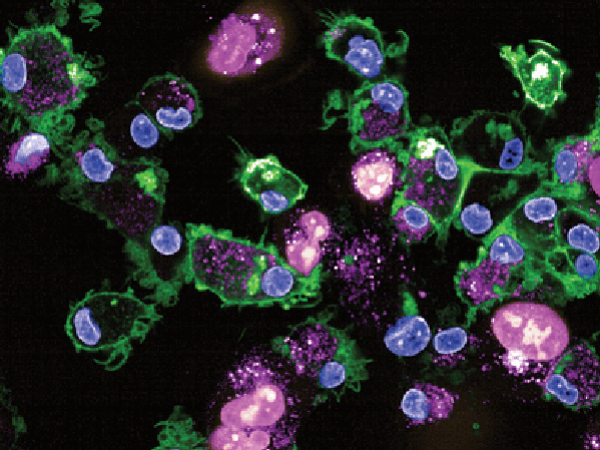
Journal: Cancer Immunology Research
Natural killer (NK) cells are important components of the innate immune response and hold promise for adoptive cellular immunotherapy, especially for the treatment of hematological malignancies. NK-cell engagers (NKCE) are molecules engineered to tether NK cells to cancer cells by engaging the NK-cell receptor CD16A and tumor-associated antigens. The authors of this study tested the in vitro effect of different NKCEs that engage CD16A along with the NK activating receptors NKp46 or NKp30 and target either CD19 or CD20 to induce killing of pediatric B-cell precursor acute lymphoblastic leukemia (BCP-ALL) cells. Cell lines and four primary leukemias were used as target cells while resting NK cells from healthy donors and from pediatric patients after haploidentical allogeneic hematopoietic stem cell transplantation (haplo-HSCT) were used as effector cells. NK cell–resistant MHH-CALL-4 cells were efficiently killed by treatment with all NKCEs, as shown by degranulation and IFNγ production. For primary BCP-ALL blasts that don’t express CD20 and have high CD19 levels, the researchers focused on NKCEs targeting CD19 and showed that NKp46- and NKp30-based NKCEs were similarly potent at inducing NK-cell activity against primary blasts. The activating effect of NKCEs was able to override the inhibitory interactions mediated by HLA class I ligands on BCP-ALL target cells, although the strongest response was observed by alloreactive NK-cell subsets with no inhibitory HLA-specific interactions. According to the authors, these in vitro findings support the therapeutic use of NKp46/CD16A/CD19-NKCE to treat BCP-ALL in children with relapsed/refractory disease, including relapse after allogeneic HSCT.
Journal: Blood Cancer Discovery
Despite the success of CD19-directed chimeric antigen receptor (CAR) T-cell therapy, relapses occur in approximately 50 percent of B-lymphoblastic leukemia (B-ALL) patients treated with this type of immunotherapy. CD22 has emerged as an alternative to CD19 as a target antigen, and anti-CD22 CAR T cells have been successful in inducing B-ALL remission, although a significant proportion of patients eventually relapse due to down-regulation of CD22 expression by mechanisms that are poorly understood. In this study, the authors studied the role played by aberrant splicing. Comparing RNA-sequencing data from a cohort of pediatric B-ALL samples and normal B cells from healthy donors, they identified several CD22 splicing variations associated with B-ALL, including a splice isoform that lacks exons 5 and 6 (Δex5–6) but produces a functional protein, which was associated with resistance to CAR T cells targeting a specific domain of the CD22 protein. The researchers also described splice variants skipping exon 2 that failed to produce any protein, thereby representing a mechanism of CD22 epitope downregulation. In line with this observation, forcing exon 2 skipping resulted in reduced CD22 protein expression and resistance to the CD22-directed antibody–drug conjugate inotuzumab ozogamicin in vitro. The authors also analyzed bone marrow and peripheral blood samples from pediatric B-ALL patients treated with inotuzumab ozogamicin in a clinical trial. In the leukemic blasts from a patient who did not respond to therapy, Δex2 isoforms comprised the majority of CD22 transcripts; in another patient, increase in exon 2 skipping caused downregulation of CD22 protein expression during relapse. While the inotuzumab-resistant CD22 isoforms were present to some degree in patient samples collected before inotuzumab ozogamicin therapy, the authors also observed new mutations that affected CD22 splicing in post-treatment samples. The presence of preexisting drug-resistant isoforms suggested that some patients may be predisposed to becoming resistant to inotuzumab ozogamicin and that this might represent a predictive biomarker of resistance. This study highlighted the importance of aberrant CD22 splicing in antigen escape from immunotherapy for B-cell malignancies. This article was highlighted in the March issue and a related commentary can be found here.
Journal: Cancer Discovery
Mutations in the isocitrate dehydrogenase 1 (IDH1) gene are frequently found in different cancer types, including cholangiocarcinoma. The mutant IDH1 (mIDH1) enzyme generates the (R)-2-hydroxyglutarate metabolite that inhibits a range of enzymes involved in different biological process, impacting epigenetics and metabolism. The authors of this study generated genetically engineered mouse models to dissect the functions of mIDH1 in the pathogenesis of intrahepatic cholangiocarcinoma. They found that mIDH1 promotes immunoevasion through a dual mechanism: suppression of CD8+ T-cell activity and inhibition of TET2, an epigenetic enzyme that has been implicated in regulating the immune response, in tumor cells. Pharmacologic mIDH1 inhibition stimulated CD8+ T-cell recruitment and interferon γ (IFNγ) expression. TET2 mediated the tumor cell response to mIDH1 inhibition by activating IFNγ target genes, as tumor cell–specific ablation of TET2 caused treatment resistance. Furthermore, CTLA4 blockade synergized with mIDH1 inhibition by overcoming IFNγ-induced checkpoint activation that leads to immune suppression. These findings shed light on the mechanism of action of mIDH1 inhibition and suggest a novel combination strategy to potentiate its efficacy. This study was featured in a commentary and on the cover of the March issue.
Journal: Molecular Cancer Therapeutics
Histone deacetylase (HDAC) inhibitors have been approved for the treatment of certain lymphomas and multiple myeloma, but challenges related to potency, selectivity, and oral bioavailability have limited their use in solid tumors. In this study, the authors sought to clinically optimize an analog of the HDAC inhibitor largazole, called OKI-006, which inhibits class I, IIb, and IV HDACs. To improve drug delivery, the researchers designed two OKI-006 prodrugs requiring biochemical activation. The prodrug optimized for use in cell cultures, OKI-005, decreased proliferation and induced apoptosis of several cell lines of colorectal cancer and triple-negative breast cancer. OKI-005 also effectively decreased tumor burden and metastasis when these cells were injected into mice. The researchers additionally developed OKI-179, optimized for use in animal models and humans. OKI-179 also resulted in a significant tumor growth reduction in mice, an effect that was compounded by cotreatment with the antiestrogen tamoxifen (Soltamox) in estrogen receptor-positive breast cancer cell xenografts. The authors of this study have used this preclinical data to launch a phase I clinical trial of OKI-179 in patients with solid tumors. This study was highlighted in and featured on the cover of the March issue.
Journal: Cancer Prevention Research

Watercress is a cruciferous vegetable rich in gluconasturtiin, the precursor of phenethyl isothiocyanate (PEITC), which has chemopreventive activity by inducing the function of several enzymes involved in the metabolism of carcinogens. This study reports on a partnership between academia and the food industry to prepare a beverage containing freeze-dried watercress to use in an ongoing chemoprevention clinical trial designed to test whether daily consumption of watercress can increase the detoxification of common environmental toxicants and carcinogens. The study is planned for 400 participants divided in two groups: one group will receive the watercress-containing drink while the other group will receive a control maltodextrin drink, and both drinks will be consumed three times daily for two weeks. After a 4-week washout period, each participant will switch to the other drink for a second 2-week period. The researchers will measure the urinary levels of a biomarker of exposure to benzene, acrolein, crotonaldehyde, and 1,3-butadiene at baseline and periodically throughout the study. According to the authors, their method for the industrial-scale production of freeze-dried watercress to prepare a PEITC-containing beverage and a positive outcome of their study would support the use of watercress for chemoprevention. This article was featured on the cover of the March issue and in a commentary that can be found here.
Journal: Cancer Research (March 1 issue)
Patients with clear cell renal cell carcinoma (ccRCC), a type of kidney cancer, are frequently treated with immunotherapy, but few biomarkers of tumor response are available. One crucial component of the tumor immune response is the ability for T-cell and B-cell receptors to recognize tumor antigens, a process that depends on a variable domain in these receptors called complementarity determining region 3 (CDR3). The authors of this study hypothesized that an increased diversity of CDR3 sequences may enable immune cells to recognize more antigens, potentially indicating improved tumor immune infiltration and response to immunotherapy. The researchers applied a series of measurements commonly used in ecology and evolution, called the generalized diversity index (GDI), to assess various scales of CDR3 diversity and attempted to correlate these measurements with clinical outcomes. The researchers sequenced tumor RNA from three different cohorts totaling 656 ccRCC patients. They found that a specific diversity metric included in the GDI—richness, or the number of unique sequences identified for each receptor—had a positive correlation with larger, more aggressive tumors. Another diversity metric—evenness, or the similarity of counts among each detected sequence—had a positive correlation with improved survival. These associations were especially strong for the CDR3 region of T-cell receptor alpha. The authors suggest that these measurements will enhance the field’s understanding of tumor-immune interactions and the ways in which these interactions influence patient outcomes. A related commentary can be found here.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Cancer mortality rates in the U.S. vary by race/ethnicity and sex, with non-Hispanic Black males experiencing the highest burden. Early detection is critical in reducing cancer mortality, as the risk of cancer death is lower when it is diagnosed and treated before metastatic spreading occurs. This study assessed the potential benefits of improved detection before metastasis for eight population subgroups defined by race/ethnicity (non-Hispanic white, non-Hispanic Black, non-Hispanic Asian/Pacific Islander, Hispanic) and sex (male, female), based on stage- and cancer-specific incidence and survival data from the Surveillance, Epidemiology, and End Results Program for persons aged 50 to 79 years, between 2006 and 2015. For each cohort, the authors estimated the incidence of cancer-related deaths if the cancers diagnosed at stage IV were detected at earlier stages. According to study results, diagnosing all stage IV cancers when they were at stage III would have resulted in a 13-14 percent reduction in cancer-related deaths across subgroups, while diagnosing one third of metastatic cancers at earlier stages would have resulted in a 21–23 percent reduction. Non-Hispanic Black experienced the highest burden of stage IV cancer and would have the most deaths averted through earlier detection. According to the authors, this study indicates that diagnosing cancer before it metastasizes could significantly reduce mortality in all populations, but especially in non-Hispanic Black populations. This article was highlighted in the March issue and a related commentary can be found here.
Journal: Clinical Cancer Research (March 1 issue)
Kaposi sarcoma is caused by the Kaposi sarcoma herpes virus (KSHV) and is more commonly diagnosed in individuals with HIV. The virus is known to disrupt antigen presentation—the process by which infected or cancerous cells signal to the immune system—dampening immune responses against the resulting tumor. While Kaposi sarcoma is often treated with chemotherapy, some tumors do not respond, and treatment can cause significant adverse events. The immunomodulatory drug pomalidomide (Pomalyst) has been shown in preclinical models to reverse the immunosuppressive effects of KSHV, and preliminary results from a phase I/II clinical trial indicated that it was safe and effective against Kaposi sarcoma in individuals with and without HIV. In this study, the researchers reported long-term efficacy and survival data from the trial. Among the 28 patients enrolled, including 18 patients with HIV, the overall response rate was 71 percent with a median response duration of 9.2 months and a median progression-free survival of 10.2 months. The subset of patients with HIV had an overall response rate of 67 percent with a median response duration of 11.3 months and a median progression-free survival of 10.3 months. Upon progression, four previously responsive patients received a second course of pomalidomide, resulting in two partial responses and two incidences of stable disease. Neutropenia and other hematological toxicities were the most common adverse events. The authors suggest that pomalidomide shows promise as a chemotherapy-sparing treatment for patients with Kaposi sarcoma. This study was highlighted in the March 1 issue.