Editors Share Highlights from September Issues of AACR Journals
As we unpack our cardigans in anticipation of cooler weather here on the East Coast, we are taking a look back at some of the highlights from the September issues of the AACR journals. In September, the editors chose to feature new developments in drug design, insights into how cancer cells respond to iron availability, and analyses of racial/ethnic disparities, coinciding with the 15th AACR Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved.
Read a brief synopsis of each highlighted study below. For more, be sure to follow the links to the full articles and published commentaries. As always, these articles will be freely available online for a limited time.
Journal: Blood Cancer Discovery
Transcriptional Plasticity Drives Leukemia Immune Escape
Patients with acute myeloid leukemia (AML) at higher risk of relapse after chemotherapy receive allogeneic bone marrow transplantation. Relapse after allogeneic bone marrow transplantation has been linked to immune evasion through loss of expression of major histocompatibility complex class II (MHCII) genes, but the mechanisms are not understood. In this study, the authors developed a computational algorithm called CORENODE to analyze the transcriptional network of AML cells. Through this approach, they identified four key transcription factors (IRF8, MYB, MEF2C, and MEIS1) that regulate MHCII expression in AML cells independently of the canonical IFNγ/CIITA pathway, with MYB and IRF8 playing major antagonistic functions. The analysis suggested that immune escape through MHCII loss may be orchestrated by combinatorial fluctuations in the abundance of the transcription factors in the tetrad. In addition, MYB and IRF8 regulated other genes involved in antigen presentation, cytokine response, and T-cell co-stimulation, resulting in reduced expression of these genes at relapse. Single-cell transcription analysis of patient samples at diagnosis and post-allogeneic stem cell transplantation showed that AML cells with low MHCII expression and altered transcription factor abundance were present at diagnosis, and, according to the authors, could be positively selected during relapse. This article was highlighted in the September issue and featured on the cover.
Journal: Cancer Discovery
Ferritinophagy is a form of selective autophagy that degrades intracellular ferritin, the major iron-storage protein in the body, resulting in the release of bioavailable iron. In this issue, two studies uncovered the role of ferritinophagy favoring survival and therapy resistance in pancreatic ductal adenocarcinoma (PDAC). The first study focused on the nuclear receptor coactivator 4 (NCOA4), which mediates ferritinophagy by targeting ferritin to the lysosome for degradation. The authors found that NCOA4-mediated ferritinophagy is upregulated in PDAC models and promotes iron metabolism and tumor progression. Furthermore, an elevated ferritinophagy gene expression signature predicted poor prognosis in PDAC patients. These results identified NCOA4-mediated ferritinophagy as a potential new therapeutic target in PDAC. The second study analyzed the mechanisms associated with metabolic adaptation of PDAC cells upon inhibition of the KRAS–MAPK pathway, which can delay tumor growth but also elicits compensatory metabolic alterations that result in the emergence of drug resistance. The authors showed that treatment of PDAC cells or patient organoids with a MEK inhibitor resulted in reduced levels of c-MYC and increased expression of autophagy and lysosomal genes mediated by the MiT/TFE transcription factor. Proteomic analysis revealed increased ferritinophagy, which resulted in enhanced mitochondrial function in response to MEK inhibition. Suppression of ferritinophagy synergized with MEK inhibition and blocked PDAC growth, pointing to a metabolic dependency that could be targeted to sensitize PDAC cells to KRAS/MAPK inhibition. These studies were featured on the cover of the September issue, and a related commentary is available here.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Hyperinsulinemia and inflammation link diet with risk of several cancers, including prostate cancer. The authors of this study investigated whether post-diagnostic behaviors that affect inflammation and the insulin pathway led to worse outcomes among patients diagnosed with nonmetastatic prostate cancer in the Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) cohort. They studied the association of prostate cancer progression and mortality with four empirically derived indices that allow for the assessment of the inflammatory and insulinemic potential of diet and lifestyles and can be used as proxies for biomarker data: empirical dietary inflammatory pattern, empirical dietary index for hyperinsulinemia, empirical dietary index for insulin resistance, and associated lifestyle indices for hyperinsulinemia and insulin resistance. Over a median follow-up of 6.4 years following a prostate cancer diagnosis, these indices were positively associated with an increased risk of disease progression. No association was observed with prostate cancer–specific mortality. These findings suggest that curbing inflammation and insulin hypersecretion through diet and an active lifestyle may improve prostate cancer survivorship. This article was highlighted in the September issue, and a related commentary is available here.
Journal: Cancer Immunology Research
Chimeric antigen receptor (CAR) T-cell therapy targeting the CD19 antigen is a major breakthrough in the treatment of CD19+ B-cell acute lymphoblastic leukemia (B-ALL); however, a considerable fraction of patients eventually experience disease relapse associated with loss of CD19 expression via different mechanisms. Using single-cell approaches, the authors of this study reported that direct interaction between CAR T cells and leukemic cells resulted in rapid clustering of B-ALL cells and internalization of CD19. Furthermore, a subset of leukemic cells maintained reduced CD19 expression by utilizing transcriptional programs characteristic of physiologic B-cell activation and germinal center reaction. Inhibition of Bruton’s tyrosine kinase (BTK), which is essential for normal B-cell activation, with ibrutinib increased the cytotoxicity of CD19 CAR T cells. According to the authors, these finding indicate that transcriptional plasticity may allow B-ALL cells to escape CAR T-cell therapy by actuating B-cell activation and germinal center reaction programs, and that combining CAR T-cell therapy with other targeted therapies may provide a strategy to overcome the plasticity of leukemic cells.
A commentary related to this article is available here.
Journal: Cancer Prevention Research
Individuals with Lynch syndrome have a heightened risk of several cancers, including those of the colon/rectum, ovary, endothelium, skin, and stomach, among others. Researchers have proposed that dietary fiber may lower colorectal cancer risk in patients with Lynch syndrome due to the production of certain metabolites and changes to the gut microbiota. In this article, the authors report results from a 10-year follow-up of the CAPP2 trial on the long-term impacts of resistant starch (a source of dietary fiber that is found in foods such as bananas, potatoes, and grains) on cancer incidence in individuals with Lynch syndrome. In the trial, participants were randomly assigned to receive either 30 grams of resistant starch or placebo daily. The latest analysis showed that there were no differences in colorectal cancer incidence between those who were given daily resistant starch and those who were given placebo; however, participants receiving daily resistant starch had significantly fewer cases of other cancer types and a 48 percent lower risk of developing these cancers compared with those receiving placebo. The authors propose daily intake of resistant starch as a potential strategy to reduce non-colorectal cancer risk in patients with Lynch syndrome. This article was featured on the cover of the September issue. A related commentary can be found here.
Journal: Cancer Research (September 1 issue)
When prostate cancer metastasizes to bone, it can mediate the transformation of endothelial cells into osteoblasts, which support metastatic tumor growth by producing additional bone. Because activation of retinoic acid receptor gamma (RARγ) has shown clinical efficacy in the treatment of genetic diseases associated with bone overproduction, the authors of this study hypothesized that RARγ signaling may also contribute to osteoblast production in the metastatic microenvironment. They found that a RARγ agonist significantly inhibited the endothelial-to-osteoblast transition in cell lines and the development of bone metastases in prostate cancer cell xenograft mouse models. The researchers discovered that RARγ likely forms a complex with BMP4, a driver of the endothelial-to-osteoblast transition, and its downstream effector SMAD1. Activated RARγ recruits the ubiquitin ligase SMURF1, which targets SMAD1 for degradation and prevents the endothelial-to-osteoblast transition. The researchers also presented evidence that all three RAR isoforms, including RARα and RARβ, are necessary for the endothelial-to-osteoblast transition, and that all-trans retinoic acid, which activates all RAR isoforms, also prevents the transition. The authors suggest that activation of RARs, especially RARγ, should be further investigated in the context of preventing prostate-to-bone metastasis. A related commentary is available here.
Journal: Cancer Research (September 15 issue)
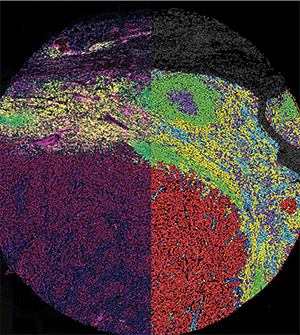
Immune checkpoint inhibitors are a common treatment for melanoma, but few biomarkers exist to predict which patients might respond. Researchers have studied how cytotoxic T cells react to immunotherapy in patients who do and do not respond to treatment, but many of these studies have not explored the spatial relationships between cells. In this study, the researchers evaluated bulk gene expression and in situ protein expression in pretreatment samples of melanoma metastases from patients who received anti-PD-1 monotherapy. The bulk gene expression identified a handful of immune-related genes and pathways differentially regulated in patients who did or did not respond to treatment. This analysis guided the selection of 87 antibodies that were applied to tumor sections to determine the identity and functional states of each cell. The researchers found that, in both patients who do and do not respond to anti-PD-1 therapy, activated cytotoxic T cells accumulate along the tumor periphery and become increasingly more exhausted and differentiated as they infiltrate the tumor. In patients who responded to treatment, macrophages expressing PD-1 colocalized with cytotoxic T cells in the tumor periphery, and macrophages adjacent to T cells had higher PD-1 expression than other macrophages. These patterns were not evident in samples from patients who did not respond. The authors suggest that spatial analyses can help researchers understand how interactions between immune cells help determine a tumor’s response to immunotherapy. This study was featured on the cover of the September 15 issue, and a related commentary is available here.
Journal: Clinical Cancer Research (September 1 issue)
Patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) who are not eligible for autologous stem cell transplantation (ASCT) have limited treatment options and a poor prognosis. The monoclonal antibody rituximab combined with the chemotherapeutic agents gemcitabine and cisplatin has been associated with a favorable safety profile. In addition, combining rituximab with the targeted therapy lenalidomide led to synergistic antitumor activity in a prior study. Based on these observations, researchers conducted a phase II clinical trial to evaluate a combination therapy consisting of rituximab, lenalidomide, gemcitabine, and cisplatin (a regimen referred to as R2-GDP) in 78 ASCT-ineligible patients with relapsed/refractory DLBCL. After a median follow-up of 37 months, 60.2 percent of patients experienced a clinical response, with 37.1 percent having a complete response and 23.1 percent a partial response. The median overall survival was 12 months, and the median progression-free survival was nine months. Among 33 patients who never had a complete response to prior therapy, the overall response rate was 45.5 percent. Common adverse events included thrombocytopenia, neutropenia, anemia, infections, and febrile neutropenia. The authors conclude that the R2-GDP combination regimen is highly active in patients with relapsed/refractory DLBCL, including in those with no prior complete responses (primary refractory). This article is highlighted in the September 1 issue. A related commentary can be found here.
Journal: Clinical Cancer Research (September 15 issue)
Medulloblastoma, neuroblastoma, Ewing sarcoma, and alveolar rhabdomyosarcoma are aggressive tumors that originate from embryonic tissue and typically affect infants and young children. Placental growth factor (PlGF) is a common driver of these tumors, and TB-403, a PlGF blocking antibody, has been shown to inhibit the growth of medulloblastoma cell lines and mouse models. In this phase I clinical trial, the researchers treated 15 patients with relapsed or treatment-refractory medulloblastoma, neuroblastoma, Ewing sarcoma, or alveolar rhabdomyosarcoma with 20 mg/kg, 50 mg/kg, 100 mg/kg, or 175 mg/kg of TB-403. Across all dose levels, only one patient experienced dose-limiting toxicities, and the maximum tolerated dose was not reached. No patients experienced partial or complete responses, but 64 percent of patients with medulloblastoma experienced stable disease, with 57 percent of those responses lasting longer than 100 days. After the first cycle of TB-403 monotherapy, patients had the option to add etoposide or temozolomide chemotherapy to their treatment regimen, and five of the seven patients with medulloblastoma who experienced stable disease received chemotherapy. The researchers recommend 175 mg/kg as an appropriate dose for a phase II trial of patients with medulloblastoma. This article was highlighted in the September 15 issue.
Journal: Molecular Cancer Research
Ceramide kinase (CERK) has been implicated as a protumorigenic enzyme, but the mechanisms underlying its protumor functions remain unclear. Here, researchers studied the role of CERK in non-small cell lung cancer (NSCLC). They observed that CERK inhibition or depletion led to greater cell death in KRAS-mutated NSCLC as compared with NSCLC with wild-type KRAS. Further experimentation revealed that inhibition of CERK led to ferroptosis in KRAS-mutated NSCLC and that this effect was dependent on the elevation of voltage-dependent anion channel (VDAC)-regulated mitochondria membrane potential and the production of reactive oxygen species. This occurred through suppression of AKT activation and mitochondrial translocation, which affected the mitochondrial membrane potential by preventing VDAC phosphorylation and tubulin recruitment. Furthermore, the authors found that adding CERK inhibition to cisplatin treatment led to a synergistic decrease in cell survival and in vivo tumor growth. According to the authors, these findings may have implications for improving precision medicine for KRAS-mutated NSCLC. This article is highlighted in the September issue.
Journal: Molecular Cancer Therapeutics
Antibody-drug conjugates (ADCs) are a form of cancer therapy designed to deliver a cytotoxic agent to cancer cells while sparing normal cells. This cancer-selective targeting is accomplished by conjugating the cytotoxic agent to antibodies that recognize an antigen expressed on the surface of cancer cells. In many existing ADCs, the cytotoxic agent is joined to the antibody via a linker made of valine and citrulline; however, the instability of valine-citrulline linkers often leads to adverse effects such as neutropenia and hepatotoxicity. In this article, researchers examined the potential of a linker made of glutamic acid, glycine, and citrulline (EGCit) to improve ADCs. They found that ADCs developed using the EGCit linker were stable in mouse and primate plasma and avoided degradation of differentiating human neutrophils without compromising the ability to deliver the cytotoxic agent into cancer cells. When compared with the FDA-approved ADCs trastuzumab emtansine (Kadcyla) and fam-trastuzumab deruxtecan-nxki (Enhertu), the EGCit-based ADC had improved antitumor activity in cancer cell lines and mouse models and showed no significant myelosuppression or liver toxicity in mice. The authors propose the EGCit linker technology as a potential approach to improve the efficacy and safety of ADCs.
Journal: Cancer Research Communications
Patients with Lung Cancer of Different Racial Backgrounds Harbor Distinct Immune Cell Profiles and
In recognition of the 15th AACR Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved, Cancer Research Communications has selected two editors’ picks this month, both discussing differences in tumor immune responsiveness among different races. In the first study, the researchers investigated whether differences in tumor immune cell distribution could explain differences in lung cancer survival rates between white and Black Americans. They found that tumors from white patients had significantly increased infiltration of CD4+ and CD8+ T cells compared with tumors from Black patients. These differences were largest among those who were current smokers and those who have never smoked but were not significant among those who previously smoked. Additionally, the researchers found that in white patients, immune cells were more likely to colocalize with cancer cells than in Black patients, in whom immune cells and tumor cells were, on average, separated by a greater distance. In the second study, the researchers retrospectively assessed how response rates to immune checkpoint inhibitors (ICI) differed among patients of different racial and ethnic groups with lung cancer or head and neck squamous cell carcinoma (HNSCC). They analyzed data from 207 patients and found that the overall response rate trended lower for Hispanic patients compared with white and Black patients. The difference in response rates was larger among patients who received ICI monotherapy as compared to those who received ICI in combination with chemotherapy. Hispanic patients also experienced fewer immune-related side effects than Black or white patients. The authors of both articles suggest that further research into the molecular mechanisms underlying differences in immune responsiveness may help understand disparities in immunotherapy success and may help better direct treatment strategies in the future.