FDA Approvals in Oncology: January-March 2023
With the approval of new anticancer therapeutics, more treatment options become available for patients. Some therapies are new to the market, while some may have already been approved for other indications; some molecules are first in class, directed against a previously untargeted pathway or acting through a new mechanism, while others may be improved versions of drugs that already exist.
To help our readers keep track of the cancer therapies approved by the U.S. Food and Drug Administration (FDA), make sense of their impact for patients, and put them in context of the current therapeutic landscape, Cancer Research Catalyst is launching a new blog series that will present a quarterly review of the latest from the FDA.
Approvals issued from January to March 2023 included targeted therapies for B-cell malignancies, colorectal cancer, and pediatric brain cancer; additional options for hormone receptor (HR)-positive breast cancers; a new immune checkpoint inhibitor; and expanded indications for previously approved immune checkpoint inhibitors.
Expanding the portfolio of targeted therapies for B-cell malignancies
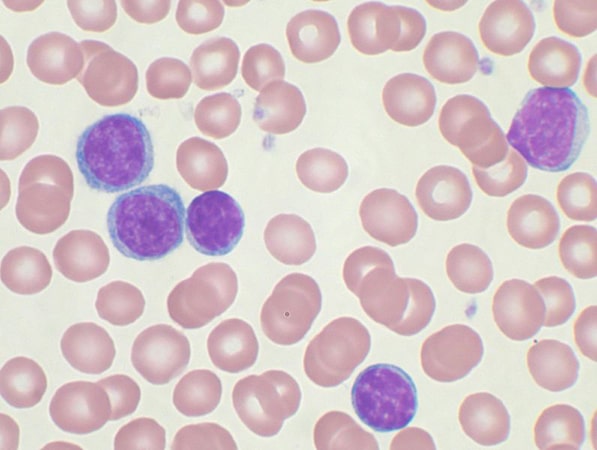
The development of molecularly targeted therapies has led to dramatic improvements in the care of patients with B-cell malignancies. Among these developments are Bruton’s tyrosine kinase (BTK) inhibitors, which block the function of the BTK enzyme that is involved in the survival of malignant B cells. The first BTK inhibitor, ibrutinib (Imbruvica), was approved in 2013, and additional inhibitors have followed.
Approvals in January 2023 included an expanded approval for a next-generation BTK inhibitor and an accelerated approval for a reversible BTK inhibitor.
- The first approval of the year, on January 19, was for the BTK inhibitor zanubrutinib (Brukinsa) for chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL). This drug was first approved in 2019 for the treatment of mantle cell lymphoma (MCL) and then in 2021 for marginal zone lymphoma, based, in part, on the results of a clinical trial published in the AACR journal Clinical Cancer Research.
Zanubrutinib is a next-generation BTK inhibitor designed to have higher efficacy and an improved safety profile compared to previous versions. A recent commentary in the AACR journal Cancer Discovery reviewed the clinical evidence that established the superiority of zanubrutinib to ibrutinib for the treatment of relapsed or refractory CLL and SLL.
- On January 27, another BTK inhibitor, pirtobrutinib (Jaypirca), was granted accelerated approval for the treatment of adult patients with MCL that has progressed following previous lines of therapy, including other BTK inhibitors. Pirtobrutinib is new to the market and is the only FDA-approved reversible BTK inhibitor, which means that it does not form a permanent bond with the BTK enzyme. Irreversible BTK inhibitors can lead to treatment resistance due to mutations in the portion of BTK that binds the inhibitor, therefore they cannot be used successively to treat patients. Pirtobrutinib was designed to remain active in the presence of acquired mutations and can be used after disease progression following treatment with existing BTK inhibitors, extending the benefit of targeting this pathway.
Targeting HER2 in colorectal cancer
On January 19, the FDA granted accelerated approval to the drug tucatinib (Tukysa) in a new combination regimen for certain patients with unresectable or metastatic colorectal cancer that has progressed following chemotherapy, a patient population that typically has limited treatment options.
Tucatinib is a small molecule inhibitor of the HER2 receptor, whose overexpression leads to tumor cell proliferation, invasion, and metastasis. The first report of the preclinical activity of tucatinib in solid tumor models was published in the AACR journal Molecular Cancer Therapeutics, and tucatinib was later approved as a breast cancer treatment for patients with HER2-positive tumors.
HER2 overexpression is found in approximately 3 to 5% of metastatic colorectal cancer. The latest indication for tucatinib extends its use to patients with HER2-positive unresectable or metastatic colorectal cancer in combination with the HER2-targeted monoclonal antibody trastuzumab (Herceptin).
More therapeutic options for patients with hormone receptor-positive breast cancer
Approvals issued in this first quarter expanded the armamentarium of therapies for estrogen receptor (ER)-positive breast cancer, including a new hormone therapy and two targeted therapies.
- Hormone therapy is used as a treatment for ER-positive breast cancer to inhibit estrogen production or block its effects on cancer cells. On January 27, elacestrant (Orserdu) was approved for certain patients with locally advanced or metastatic ER-positive, HER2-negative breast cancer.
Elacestrant belongs to a class of hormone therapy drugs called selective ER degraders (SERDs), which block ER signaling by causing degradation of the receptor. Prior to the approval of elacestrant, fulvestrant (Faslodex) was the only approved SERD, which meant patients who stopped benefiting from fulvestrant were left with few treatment options. Unlike fulvestrant, which can only be given as an intramuscular injection, elacestrant can be administered orally.
The approval of elacestrant was based on the results of a clinical trial presented in 2021 at the San Antonio Breast Cancer Symposium (SABCS), co-organized by the AACR.
- On February 3, the FDA greenlighted sacituzumab govitecan-hziy (Trodelvy) for patients with locally advanced or metastatic hormone receptor (HR)-positive, HER2-negative breast cancer that cannot be surgically removed and who have already received certain therapies. This approval expands on the 2020 approval of sacituzumab govitecan-hziy for metastatic triple-negative breast cancer.
Sacituzumab govitecan-hziy is an antibody-drug conjugate, a type of therapeutic consisting of a monoclonal antibody linked to a toxic payload. When the antibody portion binds its target protein on cancer cells, the toxic payload is internalized and kills the cancer cells with no or minimal harm to healthy cells. According to a study published in Molecular Cancer Therapeutics, the increased efficacy of sacituzumab govitecan-hziy compared to other similar drugs comes from its ability to efficiently penetrate tumors and rapidly release its payload after entering cells.
- On March 3, abemaciclib (Verzenio) was approved in combination with endocrine therapy for patients with HR-positive, HER2-negative, early breast cancer who have a high risk of disease recurrence after surgery.
Abemaciclib is a targeted therapy that inhibits the function of two cell cycle-regulating proteins, CDK4 and CDK6. Besides abemaciclib, approved CDK4/6 inhibitors include palbociclib (Ibrance) and ribociclib (Kisqali).
CDK4/6 inhibitors have become standard of care in combination with hormone therapy for patients with metastatic HR-positive, HER2-negative breast cancer.
Abemaciclib was previously approved to treat progressive (2017) or untreated (2018) advanced HR-positive, HER2-negative breast cancers. In 2021, abemaciclib was approved as adjuvant treatment for early HR-positive, HER2-negative breast cancers with a high risk of recurrence as determined by expression of the Ki-67 biomarker.
The latest approval eliminated the Ki-67 testing requirement, expanding abemaciclib use to a broader patient population. Eligibility for this therapy is now based on the number of cancer-containing lymph nodes, tumor size, and tumor grade.
The expanded indication is based on a four-year follow-up of the phase III clinical trial that led to the 2021 approval of abemaciclib for certain early breast cancers. Results from this trial were presented at SABCS in 2020.
Immunotherapy for lung, uterine, and skin cancer
Immune checkpoint inhibitors (ICIs) release the immune system’s natural brakes to help T cells fight cancer and have become part of the standard-of-care for many cancer types.
- ICIs were first approved for non-small cell lung cancer (NSCLC) in 2015 to treat patients with advanced disease that progressed after chemotherapy. Since then, the applications of immunotherapy for lung cancer treatment have been expanded from second line to first line and from advanced to earlier stages.
On January 26, the FDA greenlighted pembrolizumab (Keytruda) for the adjuvant treatment of NSCLC following surgery and platinum-based chemotherapy. Pembrolizumab is the second immune checkpoint inhibitor approved for this indication, following atezolizumab, which was approved in 2021.
- On February 9, the FDA issued full approval of the ICI dostarlimab-gxly (Jemperli) for certain patients with recurrent or advanced endometrial cancer whose tumors have a DNA repair defect called mismatch repair deficiency (dMMR), making them more likely to respond to ICIs.
Dostarlimab-gxly had received accelerated approval for this patient population in 2021. That year, the AACR Cancer Progress Report featured the experience of an endometrial cancer survivor who benefited from dostarlimab-gxly treatment through participation in a clinical trial.
In addition to dostarlimab, another ICI used to treat advanced endometrial cancer is pembrolizumab, which was approved as a monotherapy to treat tumors with DNA repair defects and in combination with a targeted therapy for tumors without DNA repair defects.
- On March 22, the FDA granted accelerated approval to a new ICI called retifanlimab-dlwr (Zynyz) for the treatment of adult patients with metastatic or recurrent locally advanced Merkel cell carcinoma, a rare but aggressive non-melanoma type of skin cancer associated with a high risk of recurrence and metastasis.
This approval expands the portfolio of ICIs approved for the treatment of Merkel cell carcinoma, which includes avelumab (Bavencio) and pembrolizumab.
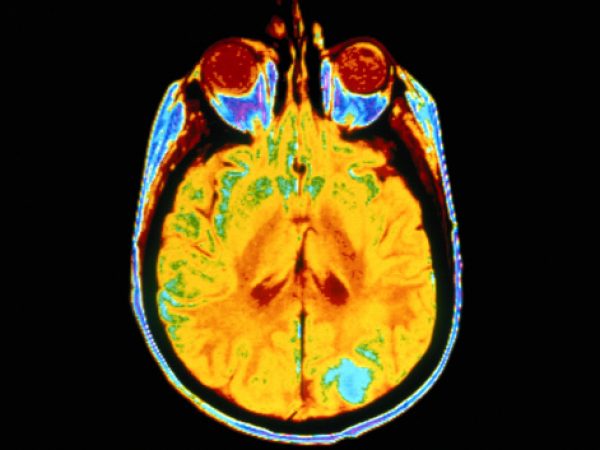
A new therapy for childhood brain cancer
On March 16, the FDA approved dabrafenib (Tafinlar) in combination with trametinib (Mekinist) for certain pediatric patients 1 year of age or older with low-grade glioma, the most common type of pediatric brain cancer.

Surgery is the mainstay of treatment for pediatric low-grade glioma, and the survival rates of patients whose tumors are completely resected is high. When complete resection cannot be achieved, or in cases where surgery is not an option, chemotherapy is used to prevent recurrence or progression, but toxicity is a concern.
The new approval marks the first targeted treatment option for patients who require systemic therapy and whose tumors harbor a specific mutation in the BRAF gene, known as V600E and associated with poor response to chemotherapy and radiotherapy.
Dabrafenib and trametinib are molecularly targeted therapies that block the activity of the BRAF and MEK signaling proteins, respectively, to shut down the signaling pathway that is commonly activated in tumors with BRAF mutations.
This combination was previously approved for patients 6 years of age and older with BRAF V600E-mutated unresectable or metastatic solid tumors, including low-grade glioma, that had progressed following prior therapy.
For more details, including the full indications and the clinical trial results that led to each approval, visit the FDA approvals page on the AACR website.