AACR Annual Meeting 2023: Designing, Targeting, and Delivering Novel Cancer Drugs
The era of targeted cancer therapy has fundamentally transformed the way several cancers are treated and has provided new avenues to patients with limited options.
Nevertheless, researchers in the targeted therapy field aren’t resting on their laurels. Challenges in target identification, drug design, and drug delivery limit the current applications of targeted therapies, and experts are working to design creative ways to overcome these hurdles.
The fifth plenary session at the AACR Annual Meeting 2023, held April 14-19, highlighted unique advances—including new software, engineered peptides, microRNAs, and nanoparticles—that can help researchers target new proteins and tumor sites while minimizing toxicities. In the session, titled “New Concepts in Drug Discovery and Engineering,” experts presented new drug design applications that could help shape the next generation of cancer therapeutics.
Identifying New Drug Targets
According to the National Cancer Institute, only 15% of proteins are currently considered druggable.
However, the recent success of inhibitors targeting the previously undruggable KRAS has driven scientists to rethink the contours in a protein’s surface that determine its druggability, according to Gregory Bowman, PhD, a professor of bioengineering, biochemistry, and biophysics at the University of Pennsylvania and director of Folding@home.
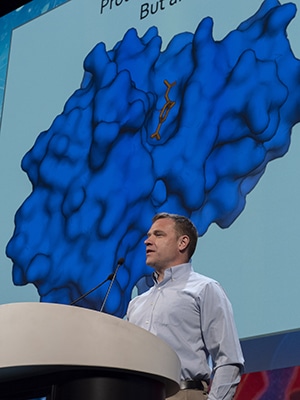
Computer simulations can help researchers better understand the shape of proteins as they fold into their mature form or vacillate between states and predict if the proteins have cryptic pockets—those that only exist during transient protein states—where drugs can bind.
“I have a very different intuition for proteins as molecular machines that are full of moving parts that aren’t obvious from the single structures that we’re familiar with,” Bowman said. “If we could watch the sorts of dynamics that this folded protein undergoes, we would have the opportunity to identify these pockets prospectively and intentionally target them.”
Such simulations require a significant amount of time and computing power to run, making it difficult to rapidly interrogate multiple proteins. To address this hurdle, Bowman has founded Folding@home, an international consortium that recruits citizens to download software to their computer that allows research labs running folding simulations to use part of these individuals’ idle CPU power.
A separate software program, called PocketMiner, interrogates each residue in a protein structure and calculates the probability that it could form part of a cryptic pocket. Researchers can overlay this data onto the protein’s crystal structure to visualize the putative pockets in three dimensions. Preliminary data estimated that over half of supposedly undruggable proteins may have a cryptic pocket.
“Maybe you should reconsider the viability of going after some of the targets that you might have shied away from,” Bowman said.
Advances in Antibody-drug Conjugates
In recent years, antibody-drug conjugates (ADCs), which use an antibody to deliver toxic compounds directly to cancer cells, have emerged as a popular option to target proteins on the cell surface.

As researchers develop new generations of ADCs, they learn more about how to maximize efficacy, minimize toxicity, and overcome resistance, explained Puja Sapra, PhD, senior vice president of biologics engineering and oncology targeted delivery at AstraZeneca. “We have to move away from empirical drug design and development for ADCs to rational drug design,” Sapra said, explaining that all components of an ADC should be optimized to match the drug target and tumor type.
This starts with the selection of an appropriate target, Sapra continued. To minimize toxicity, an ideal ADC target should be abundantly expressed and efficiently internalized into cancer cells but not normal cells. The repertoire is limited, but Sapra suggested that bispecific ADCs—targeting proteins that are coexpressed only on cancer cells—may circumvent this problem.
For example, Sapra and colleagues are developing a bispecific antibody targeting both EGFR and c-MET. In patient-derived xenograft mouse models of various solid tumors, the antibody effectively decreased tumor growth regardless of whether the tumors harbored EGFR mutations.
Sapra also emphasized the importance of a cleavable linker that will release the drug only when inside tumor cells. She highlighted site-specific conjugation, in which researchers engineer the antibody with moieties that hold their drug with high affinity, rather than relying on native lysines and cysteines.
In terms of payload selection, Sapra said that “the future possibilities are endless,” when it comes to optimizing payloads for each scenario. For example, a tumor’s response to an ADC could depend on its sensitivity to the payload as much as its expression of the antibody target. Sapra suggested that studies evaluating biomarkers of payload sensitivity could help predict a patient’s response to an ADC.
New Peptide-based Therapies
While antibody-based therapies have transformed the landscape of cancer treatment, there are situations they cannot address, explained Jennifer Cochran, PhD, senior associate vice provost for research, a professor of bioengineering, and a professor by courtesy of chemical engineering at Stanford University.

“Antibodies have some limitations that other types of proteins can help solve,” Cochran said. For example, antibodies aren’t adept at disrupting high-affinity interactions, such as the one between oncogenic Axl and its ligand Gas6. Cochran and colleagues sought to design a small peptide—a decoy of the Axl receptor—that bound more tightly to Gas6 than the endogenous receptor.
Their first-generation molecule bound to Gas6 with an affinity of 400 femtomolar and decreased ovarian cancer metastasis in a mouse model by 90%. Their second-generation molecule bound with an affinity of 90 femtomolar and decreased metastatic spread by 99%. The latter is currently being evaluated in a phase III clinical trial for patients with platinum-resistant ovarian cancer and in earlier phase trials for patients with kidney and pancreatic cancer.
Cochran showed that peptide-drug conjugates (PDCs) may also have certain advantages over ADCs, including their small size, which allows them to diffuse deeper into the tumor tissue. She and her colleagues designed a peptide called PIP, which targets a specific conformation of integrin proteins found on the surface of cancer cells.
The researchers tested PIP-based applications, including a PDC and an ADC. Cochran and colleagues found that the PDCs penetrated deeper into spheroid models than the ADCs. In a mouse glioma xenograft model, the PDC significantly decreased tumor growth compared to the ADC.
“If you have something that’s really small, and it has very high affinity, you can be in this sweet spot of good extravasation and really robust tumor uptake,” Cochran said. “This is where we’re at with our PIP molecule.”
miCrO-RNA as a Cancer Drug
Scientists have been using microRNAs (miRNAs)—small RNAs that target specific messenger RNA sequences for degradation—to silence genes in cancer models since their discovery in the early 1990s. Andrea Kasinski, PhD, an associate professor of biological sciences at Purdue University, explained that the successful use of miRNAs in a cancer patient presents additional challenges.
“The first thing is that you’ve got to get the RNA to the cell of interest, and that’s not trivial,” Kasinski said. “Then, we’re challenged with getting it into the cell, and not just into the cell but into the correct bioactive compartment.”
Researchers have tried delivery vehicles such as antibodies, polymers, lipids, gold nanoparticles, and viruses, but they have largely been associated with high toxicity, Kasinski said. She and her colleagues hypothesized that they could do away with protective coatings, improve the targeting of the RNA, and modify the RNA itself to increase its stability.
Drawing from an FDA-approved dye that finds folate receptor-positive tumors by conjugating the dye to folate molecules, Kasinski and colleagues chemically linked folate to the miRNA miR-34a, which targets a variety of oncogene RNAs. In a mouse model of lung cancer, the miRNA conjugate effectively infiltrated the tumors and reduced their growth.
The researchers improved the stability of miR-34a with a series of chemical modifications that kept the miRNA intact for several days in cell culture without affecting its ability to degrade target genes. When they treated mouse xenograft models with the more stable miRNA conjugate, it significantly decreased tumor growth and almost completely silenced the expression of its target genes.
“This is not common for miRNA therapeutics; miRNA targeting usually results in [target RNA] downregulation of 50% if you’re lucky,” Kasinski said. “We’re bringing these [targets] down to levels we believe will be essential to use these agents in combination with other standard of care agents.”
Innovative Mechanisms of Drug Delivery
Other methods of ensuring therapies reach their target destinations include packaging them inside nanoparticles. Evan Scott, PhD, an associate professor of biomedical engineering at Northwestern University, showed how a single polymer, called polyethylene glycol-b-polypropylene sulfate (PEG-b-PPS), can form a broad library of structures capable of targeting different cell types and dodging various elements of the tumor microenvironment.

By altering the length of the polymer and the ratio of PEG to PPS, Scott and colleagues have made PEG-b-PPS into a variety of shapes, from small, micelle-like structures to large bicontinuous nanospheres to filomicelles that can form collagen-like meshes.
“We take a holistic approach,” Scott said. “Holistic is a strange term, but it means we’re taking into account every single component of the particle. We look at the size, the morphology, the surface chemistry, and the charge. How does this all matter in terms of targeting?”
For example, elongated, oval-like particles are less likely to be taken up by phagocytic immune cells. For a drug needing extra time to reach its target, bicontinuous nanospheres are stable at physiological conditions for up to 150 hours.
By modulating the surface chemistry of the nanoparticles, Scott explained, researchers can passively influence the endogenous molecules likely to stick to the nanoparticle, which can impact where the particle travels and what cells it interacts with. Alternatively, researchers can append antibodies, peptides, or other molecules onto the nanoparticle surface to direct it to cells of interest.
In a mouse model, Scott and colleagues have shown that subcutaneously injected nanoparticles show differential uptake in various tumor-associated immune cells depending on the nanoparticles’ shape, demonstrating the potential to differentially target components of the tumor immune microenvironment.
Scott concluded that, like proteins, nanoparticles are composed of modifiable parts that researchers can exploit to elicit different effects. Scott explained that understanding the broad diversity of nanoparticle structures could uncover creative solutions to problems with drug delivery.
Drug Discovery in Action
The meeting also featured a series of three sessions, hosted by the AACR Chemistry in Cancer Research working group, that highlighted 12 new drugs entering phase I clinical trials. The series, called “New Drugs on the Horizon,” covered topics including novel ADCs, targeted protein degradation technologies, and small molecule inhibitors of innovative drug targets.
View a summary of the 12 new drugs here, or registered meeting attendees can watch parts one, two, and three of the series on the virtual meeting platform.