Editors’ Picks: May Highlights from the AACR Journals
Another month brings another round of Editors’ Picks!
As we picked our May flowers, the editors picked their favorite cancer research studies published this month in the 10 AACR journals. May’s selections include an evaluation of the progress necessary to achieve the Cancer Moonshot goal, a look at cancer incidence among U.S. veterans, updated results of a phase II clinical trial in lung cancer, and more.
The abstracts of the selected studies are included below. As always, these articles are freely available for a limited time.
Journal: Blood Cancer Discovery
RNA splicing dysregulation underlies the onset and progression of cancers. In chronic lymphocytic leukemia (CLL), spliceosome mutations leading to aberrant splicing occur in ∼20% of patients. However, the mechanism for splicing defects in spliceosome-unmutated CLL cases remains elusive. Through an integrative transcriptomic and proteomic analysis, we discover that proteins involved in RNA splicing are post-transcriptionally upregulated in CLL cells, resulting in splicing dysregulation. The abundance of splicing complexes is an independent risk factor for poor prognosis. Moreover, increased splicing factor expression is highly correlated with the abundance of METTL3, an RNA methyltransferase that deposits N6-methyladenosine (m6A) on mRNA. METTL3 is essential for cell growth in vitro and in vivo and controls splicing factor protein expression in a methyltransferase-dependent manner through m6A modification-mediated ribosome recycling and decoding. Our results uncover METTL3-mediated m6A modification as a novel regulatory axis in driving splicing dysregulation and contributing to aggressive CLL.
This study was featured on the cover of the May issue, and a related commentary is available here.
Journal: Cancer Discovery
Opportunities for Achieving the Cancer Moonshot Goal of a 50% Reduction in Cancer Mortality by 2047

On February 2, 2022, President Biden and First Lady Dr. Biden reignited the Cancer Moonshot, setting a new goal to reduce age-standardized cancer mortality rates by at least 50% over the next 25 years in the United States. We estimated trends in U.S. cancer mortality during 2000 to 2019 for all cancers and the six leading types (lung, colorectum, pancreas, breast, prostate, liver). Cancer death rates overall declined by 1.4% per year from 2000 to 2015, accelerating to 2.3% per year during 2016 to 2019, driven by strong declines in lung cancer mortality (−4.7%/year, 2014 to 2019). Recent declines in colorectal (−2.0%/year, 2010–2019) and breast cancer death rates (−1.2%/year, 2013–2019) also contributed. However, trends for other cancer types were less promising. To achieve the Moonshot goal, progress against lung, colorectal, and breast cancer deaths needs to be maintained and/or accelerated, and new strategies for prostate, liver, pancreatic, and other cancers are needed. We reviewed opportunities to prevent, detect, and treat these common cancers that could further reduce population-level cancer death rates and also reduce disparities.
This study was highlighted and featured on the cover of the May issue, and a related commentary is available here. The study was discussed during a media briefing at the AACR Annual Meeting 2023, as described in a recent blog post.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Background: Prior research linking military factors with cancer-specific mortality has shown inconsistent findings, with few studies examining these associations among U.S. service members and veterans who served in Operation Iraqi Freedom/Operation Enduring Freedom conflicts.
Methods: Cancer mortality between 2001 and 2018 was ascertained from the Department of Defense Medical Mortality Registry and National Death Index for 194,689 Millennium Cohort Study participants. Cause-specific Cox proportional hazard models were used to examine links between military characteristics and cancer mortality [overall, early (<45 years), and lung].
Results: Compared with individuals who deployed with no combat experiences, non-deployers had a greater risk of overall [HR = 1.34; 95% confidence interval (CI) = 1.01–1.77] and early cancer mortality (HR = 1.80; 95% CI = 1.06–3.04). Enlisted individuals had a greater risk of lung cancer mortality compared with officers (HR = 2.65; 95% CI = 1.27–5.53). No associations by service component, branch, or military occupation and cancer mortality were observed. Higher education was associated with reduced overall, early and lung cancer mortality risk and smoking and life stressors were associated with elevated overall and lung cancer mortality risk.
Conclusions: These findings are consistent with the healthy deployer effect in which military personnel who were deployed tend to be healthier than those who did not deploy. Further, these findings highlight the importance of considering socioeconomic factors, such as military rank, that may have long-term implications for health.
Impact: These findings highlight military occupational factors that may predict long-term health outcomes. Additional work is necessary to investigate more nuanced environmental and occupational military exposures and cancer mortality.
This study was highlighted in the May issue.
Journal: Cancer Immunology Research
Low TCR Binding Strength Results in Increased Progenitor-like CD8+ Tumor-Infiltrating Lymphocytes
T-cell receptor (TCR) binding strength to peptide-MHC antigen complex influences numerous T-cell functions. However, the vast diversity of a polyclonal T-cell repertoire for even a single antigen greatly increases the complexity of studying the impact of TCR affinity on T-cell function. Here, we determined how TCR binding strength affected the protein and transcriptional profile of an endogenous, polyclonal T-cell response to a known tumor-associated antigen (TAA) within the tumor microenvironment (TME). We confirmed that the staining intensity by flow cytometry and the counts by sequencing from MHC-tetramer labeling were reliable surrogates for the TCR-peptide-MHC steady-state binding affinity. We further demonstrated by single-cell RNA sequencing that tumor-infiltrating lymphocytes (TIL) with high and low binding affinity for a TAA can differentiate into cells with many antigen-specific transcriptional profiles within an established TME. However, more progenitor-like phenotypes were significantly biased towards lower affinity T cells, and proliferating phenotypes showed significant bias towards high-affinity TILs. In addition, we found that higher affinity T cells advanced more rapidly to terminal phases of T-cell exhaustion and exhibited better tumor control. We confirmed the polyclonal TIL results using a TCR transgenic mouse possessing a single low-affinity TCR targeting the same TAA. These T cells maintained a progenitor-exhausted phenotype and exhibited impaired tumor control. We propose that high-affinity TCR interactions drive T-cell fate decisions more rapidly than low-affinity interactions and that these cells differentiate faster. These findings illustrate divergent forms of T-cell dysfunction based on TCR affinity which may impact TIL therapies and antitumor responses.
Journal: Cancer Prevention Research
Stressful Life Events, Social Support, and Incident Breast Cancer by Estrogen Receptor Status
Chronic stress affects immune function and hormonal signaling and has been hypothesized to be associated with breast cancer, although results from the few prior studies are mixed and have not examined potential differences by estrogen receptor (ER) status. Using the Women’s Health Initiative study, we included 76,951 postmenopausal women followed for events for a median of 16.7 years to investigate the association between baseline self-reported stressful life events and incident breast cancer by ER status and whether the association was modified by social support. We generated Cox proportional hazards models adjusting for demographic, clinical, lifestyle/behavioral, and social factors to estimate HRs and 95% confidence intervals (95%CI). The mean age was 63 (SD, 7.3), and majority of participants were White race (83.5%) and married or in a marriage-like relationship (63.0%). In analyses stratified by ER status, there was no relationship between stressful life events and ER-positive breast cancer. In contrast, compared with women in the lowest quartile, those in higher quartiles had an increased risk of ER-negative breast cancer, where those in quartile 4 had the highest risk (Quartile 4 vs. Quartile 1; HR = 1.30; 95%CI, 1.01–1.68; Ptrend = 0.050). Moreover, associations were stronger for the highest versus lowest quartile of stressful life events among widowed women (HR = 2.39; 95%CI, 1.29–4.44; Pinteraction<0.001). Association between stressful life events and ER-negative breast cancer was not modified by social support. In this cohort of postmenopausal women, higher experiences of prediagnostic stressful life events were associated with increased risk of ER-negative breast cancer.
Journal: Cancer Research (May 1 issue)
Advanced high-grade serous ovarian cancer (HGSC) is an aggressive disease that accounts for 70% of all ovarian cancer deaths. Nevertheless, 15% of patients diagnosed with advanced HGSC survive more than 10 years. The elucidation of predictive markers of these long-term survivors (LTS) could help identify therapeutic targets for the disease, and thus improve patient survival rates. To investigate the stromal heterogeneity of the tumor microenvironment (TME) in ovarian cancer, we used spatial transcriptomics to generate spatially resolved transcript profiles in treatment-naïve advanced HGSC from LTS and short-term survivors (STS) and determined the association between cancer-associated fibroblasts (CAF) heterogeneity and survival in patients with advanced HGSC. Spatial transcriptomics and single-cell RNA-sequencing data were integrated to distinguish tumor and stroma regions, and a computational method was developed to investigate spatially resolved ligand–receptor interactions between various tumor and CAF subtypes in the TME. A specific subtype of CAFs and its spatial location relative to a particular ovarian cancer cell subtype in the TME correlated with long-term survival in patients with advanced HGSC. Also, increased APOE-LRP5 crosstalk occurred at the stroma-tumor interface in tumor tissues from STS compared with LTS. These findings were validated using multiplex IHC. Overall, this spatial transcriptomics analysis revealed spatially resolved CAF-tumor crosstalk signaling networks in the ovarian TME that are associated with long-term survival of patients with HGSC. Further studies to confirm whether such crosstalk plays a role in modulating the malignant phenotype of HGSC and could serve as a predictive biomarker of patient survival are warranted.
A related commentary on this study is available here.
Journal: Cancer Research (May 15 issue)
Cancer-associated fibroblasts (CAF) are a major cell type in the stroma of solid tumors and can exert both tumor-promoting and tumor-restraining functions. CAF heterogeneity is frequently observed in pancreatic ductal adenocarcinoma (PDAC), a tumor characterized by a dense and hypoxic stroma that features myofibroblastic CAFs (myCAF) and inflammatory CAFs (iCAF) that are thought to have opposing roles in tumor progression. While CAF heterogeneity can be driven in part by tumor cell–produced cytokines, other determinants shaping CAF identity and function are largely unknown. In vivo, we found that iCAFs displayed a hypoxic gene expression and biochemical profile and were enriched in hypoxic regions of PDAC tumors, while myCAFs were excluded from these regions. Hypoxia led fibroblasts to acquire an inflammatory gene expression signature and synergized with cancer cell–derived cytokines to promote an iCAF phenotype in a HIF1α-dependent fashion. Furthermore, HIF1α stabilization was sufficient to induce an iCAF phenotype in stromal cells introduced into PDAC organoid cocultures and to promote PDAC tumor growth. These findings indicate hypoxia-induced HIF1α as a regulator of CAF heterogeneity and promoter of tumor progression in PDAC.
A related commentary on this study is available here.
Journal: Clinical Cancer Research (May 1 issue)
Purpose: Clinical biomarkers to identify patients unlikely to benefit from CDK4/6 inhibition (CDK4/6i) in combination with endocrine therapy (ET) are lacking. We implemented a comprehensive circulating tumor DNA (ctDNA) analysis to identify genomic features for predicting and monitoring treatment resistance.
Experimental Design: ctDNA was isolated from 216 plasma samples collected from 51 patients with hormone receptor–positive (HR+)/HER2-negative (HER2−) metastatic breast cancer (MBC) on a phase II trial of palbociclib combined with letrozole or fulvestrant (NCT03007979). Boosted whole-exome sequencing (WES) was performed at baseline and clinical progression to evaluate genomic alterations, mutational signatures, and blood tumor mutational burden (bTMB). Low-pass whole-genome sequencing was performed at baseline and serial timepoints to assess blood copy-number burden (bCNB).
Results: High bTMB and bCNB were associated with lack of clinical benefit and significantly shorter progression-free survival (PFS) compared with patients with low bTMB or low bCNB (all P < 0.05). Dominant APOBEC signatures were detected at baseline exclusively in cases with high bTMB (5/13, 38.5%) versus low bTMB (0/37, 0%; P = 0.0006). Alterations in ESR1 were enriched in samples with high bTMB (P = 0.0005). There was a high correlation between bTMB determined by WES and bTMB determined using a 600-gene panel (R = 0.98). During serial monitoring, an increase in bCNB score preceded radiographic progression in 12 of 18 (66.7%) patients.
Conclusions: Genomic complexity detected by noninvasive profiling of bTMB and bCNB predicted poor outcomes in patients treated with ET and CDK4/6i and identified early disease progression before imaging. Novel treatment strategies including immunotherapy-based combinations should be investigated in this population.
This article was highlighted in the May 1 issue.
Journal: Clinical Cancer Research (May 15 issue)
Purpose: The final analyses of the INSIGHT phase II study evaluating tepotinib (a selective MET inhibitor) plus gefitinib versus chemotherapy in patients with MET-altered EGFR-mutant non-small cell lung cancer (NSCLC) (data cut-off: September 3, 2021).
Patients and Methods: Adults with advanced/metastatic EGFR-mutant NSCLC, acquired resistance to first-/second-generation EGFR inhibitors, and MET gene copy number (GCN) ≥5, MET:CEP7 ≥2, or MET IHC 2+/3+ were randomized to tepotinib 500 mg (450 mg active moiety) plus gefitinib 250 mg once daily, or chemotherapy. Primary endpoint was investigator-assessed progression-free survival (PFS). MET-amplified subgroup analysis was preplanned.
Results: Overall (N = 55), median PFS was 4.9 months versus 4.4 months [stratified HR, 0.67; 90% CI, 0.35–1.28] with tepotinib plus gefitinib versus chemotherapy. In 19 patients with MET amplification (median age 60.4 years; 68.4% never-smokers; median GCN 8.8; median MET/CEP7 2.8; 89.5% with MET IHC 3+), tepotinib plus gefitinib improved PFS (HR, 0.13; 90% CI, 0.04–0.43) and overall survival (OS; HR, 0.10; 90% CI, 0.02–0.36) versus chemotherapy. Objective response rate was 66.7% with tepotinib plus gefitinib versus 42.9% with chemotherapy; median duration of response was 19.9 months versus 2.8 months. Median duration of tepotinib plus gefitinib was 11.3 months (range, 1.1–56.5), with treatment >1 year in six (50.0%) and >4 years in three patients (25.0%). Seven patients (58.3%) had treatment-related grade ≥3 adverse events with tepotinib plus gefitinib and five (71.4%) had chemotherapy.
Conclusions: Final analysis of INSIGHT suggests improved PFS and OS with tepotinib plus gefitinib versus chemotherapy in a subgroup of patients with MET-amplified EGFR-mutant NSCLC, after progression on EGFR inhibitors.
This article was highlighted in the May 15 issue.
Journal: Molecular Cancer Research
The Elongin BC Complex Negatively Regulates AXL and Marks a Differentiated Phenotype in Melanoma
High expression of the receptor tyrosine kinase AXL is implicated in epithelial-to-mesenchymal transition, cancer progression, and therapy resistance. For example, AXL is abundant in BRAF mutant melanomas progressing on targeted BRAF/MEK inhibition. Therefore, AXL is thought to represent an attractive therapeutic target. This notwithstanding, little is known about the mechanisms governing expression of AXL. Here, we describe a FACS-based whole-genome-wide CRISPR-Cas9 screen to uncover regulators of AXL expression. We identified several genes, inactivation of which led to increased AXL expression. Most remarkable was the identification of five components that associate with the Elongin BC heterodimer. Elongin B/C engage in multiple protein–protein interactions, including the transcription factor complex subunit Elongin A, the von Hippel-Lindau (VHL) tumor suppressor protein, and members of the SOCS-box protein family. The screen identified ELOB, ELOC, SOCS5, UBE2F, and RNF7, each of which we demonstrate to serve as an inhibitor of AXL expression. Although the AXL promoter contains hypoxia response elements and Elongin B/C are found in the VHL complex, Elongin B/C unexpectedly regulate AXL independently of hypoxia. Instead, we demonstrate that the Elongin BC complex interacts with AXL through ELOB and contributes to proteasomal AXL turnover. RNA-sequencing and IHC analyses of melanoma patient-derived xenografts and clinical samples revealed a negative association between Elongin B/C and dedifferentiation. Together, the Elongin BC complex regulates AXL and marks a differentiated melanoma phenotype.
This article was highlighted and featured on the cover of the May issue.
Journal: Molecular Cancer Therapeutics
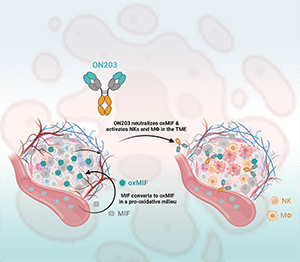
High levels of macrophage migration inhibitory factor (MIF) in patients with cancer are associated with poor prognosis. Its redox-dependent conformational isoform, termed oxidized MIF (oxMIF), is a promising tumor target due to its selective occurrence in tumor lesions and at inflammatory sites. A first-generation anti-oxMIF mAb, imalumab, was investigated in clinical trials in patients with advanced solid tumors, where it was well tolerated and showed signs of efficacy. However, imalumab has a short half-life in humans, increased aggregation propensity, and an unfavorable pharmacokinetic profile. Here, we aimed to optimize imalumab by improving its physicochemical characteristics and boosting its effector functions. Point mutations introduced into the variable regions reduced hydrophobicity and the antibodies’ aggregation potential, and increased plasma half-life and tumor accumulation in vivo, while retaining affinity and specificity to oxMIF. The introduction of mutations into the Fc region known to increase antibody-dependent cellular cytotoxicity resulted in enhanced effector functions of the novel antibodies in vitro, whereas reduced cytokine release from human peripheral blood mononuclear cells in the absence of target antigen by the engineered anti-oxMIF mAb ON203 versus imalumab reveals a favorable in vitro safety profile. In vivo, ON203 mAb demonstrated superior efficacy over imalumab in both prophylactic and established prostate cancer (PC3) mouse xenograft models. In summary, our data highlight the potential of the second-generation anti-oxMIF mAb ON203 as a promising immunotherapy for patients with solid tumors, warranting clinical evaluation.
This article was highlighted and featured on the cover of the May issue.
Journal: Cancer Research Communications
PI3K delta (PI3Kδ) inhibitors are used to treat lymphomas but safety concerns and limited target selectivity curbed their clinical usefulness. PI3Kδ inhibition in solid tumors has recently emerged as a potential novel anticancer therapy through the modulation of T-cell responses and direct antitumor activity. Here we report the exploration of IOA-244/MSC2360844, a first-in-class non–ATP-competitive PI3Kδ inhibitor, for the treatment of solid tumors. We confirm IOA-244’s selectivity as tested against a large set of kinases, enzymes, and receptors. IOA-244 inhibits the in vitro growth of lymphoma cells and its activity correlates with the expression levels of PIK3CD, suggesting cancer cell–intrinsic effects of IOA-244. Importantly, IOA-244 inhibits regulatory T cell proliferation while having limited antiproliferative effects on conventional CD4+ T cells and no effect on CD8+ T cells. Instead, treatment of CD8 T cells with IOA-244 during activation, favors the differentiation of memory-like, long-lived CD8, known to have increased antitumor capacity. These data highlight immune-modulatory properties that can be exploited in solid tumors. In CT26 colorectal and Lewis lung carcinoma lung cancer models, IOA-244 sensitized the tumors to anti-PD-1 (programmed cell death protein 1) treatment, with similar activity in the Pan-02 pancreatic and A20 lymphoma syngeneic mouse models. IOA-244 reshaped the balance of tumor-infiltrating cells, favoring infiltration of CD8 and natural killer cells, while decreasing suppressive immune cells. IOA-244 presented no detectable safety concerns in animal studies and is currently in clinical phase Ib/II investigation in solid and hematologic tumors.