A ‘Gutsy’ Approach to Predict Immunotherapy Responses
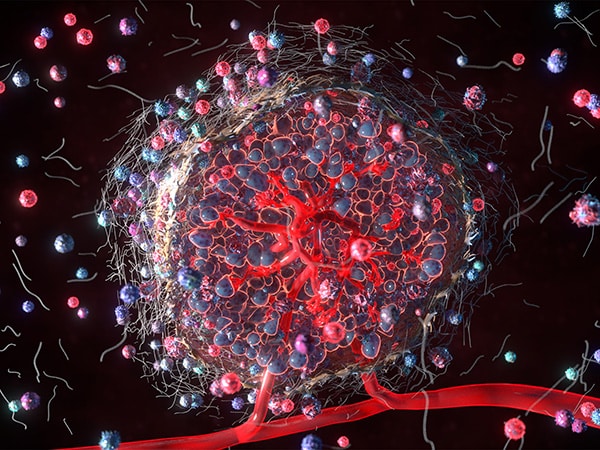
A recent study suggests that the bacteria in a patient’s gastrointestinal tract—i.e., the gut microbiome—could help clinicians make more informed decisions about immune checkpoint inhibitors (ICIs), a type of immunotherapy that boosts the immune system’s natural ability to find and attack cancers.
Given the side effects and steep costs associated with ICIs, researchers are looking for ways to figure out who is most likely to benefit so that the majority of patients whose tumors are unlikely to respond can be spared the toxicities and financial burdens of these treatments. Currently, tumor biomarkers such as high mutation burden, deficiency in mismatch repair, and expression of the immune checkpoint protein PD-L1 are used to determine eligibility for ICIs. These biomarkers, however, can be unreliable at predicting response and difficult to detect due to low or variable expression, leaving researchers in search of better methods.
One idea under exploration is to examine the gut microbiome, which has been reported to have a profound influence on the immune system. In a recent commentary published in the American Association for Cancer Research (AACR) journal Cancer Discovery, Laurence Zitvogel, MD, PhD, and Guido Kroemer, MD, PhD, from Gustave Roussy Cancer Center in France, detailed how changes to a patient’s gut microbiome—such as those caused by antibiotic use—can affect immune activity against cancer.
They explained that changes to gut bacteria can suppress the antitumor immune response and reduce the efficacy of immunotherapy due to the depletion of nutrients required for adequate immune function, fewer microbial patterns that activate immune signaling, and the loss of bacteria that can infect cancer cells and trigger an immune response within the tumor, among other mechanisms.
How Can the Gut Microbiome Guide Immunotherapy Use?
Building on this research, Zitvogel, Kroemer, and colleagues explored whether changes to a patient’s gut bacteria could provide clues about their chances of responding to immunotherapy. Earlier studies had often come to contradicting conclusions about which bacteria impacted ICI efficacy, so the researchers opted not to focus on any particular bacterial species in isolation and instead investigated the communities that gut bacteria form with one another.
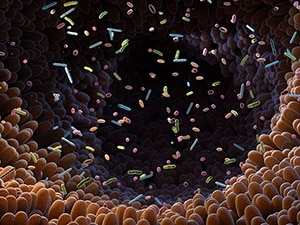
As reported in Cell, they began by sequencing fecal samples from patients with advanced lung cancer to define the bacterial species present in each patient’s gut before and during ICI treatment. By comparing the bacterial communities present in patients who did and did not experience responses to ICI treatment, they defined which bacterial communities were associated with treatment response and which were associated with treatment resistance.
The researchers categorized these communities into two “species-interacting groups” (SIGs)—SIG1, comprised of bacterial communities associated with ICI resistance, and SIG2, of communities associated with ICI response. The ratio of SIG1 to SIG2, combined with the relative abundance of the bacterium Akkermansia muciniphila, was used to calculate a topological score (termed TOPOSCORE by the authors) that estimated a patient’s likelihood of ICI response with greater accuracy than the established predictive biomarker PD-L1.
Since the type of complex genetic sequencing used to calculate TOPOSCORE is time-consuming, expensive, and not widely available, the researchers translated their method into a simplified PCR test that could be more easily implemented in the clinic. The simplified test, designed to detect 21 bacterial species instead of 83, showed comparable performance to the more complicated method across diverse cancer types.
The authors propose TOPOSCORE (in either the full or simplified form) as a clinical tool to determine patient eligibility for ICIs. Further, they speculate that TOPOSCORE could even identify patients whose chances of treatment response might benefit from interventions that modify their gut microbiomes—prebiotics or fecal transplants, for example.