Thyroid Cancer: Playing ‘Molecular Chess’ Against a Grandmaster
Despite oncologists’ best efforts to kill them, cancer cells, like all living things, tend to cling tenaciously to life. In doing so, the disease employs a fiendish array of strategies that are so complex, multifarious, and drawn out it can almost feel like practitioners are matching wits against a conscious adversary.
This has led some practitioners to liken treating cancer to a game of “molecular chess.” Oncologists mount campaigns only to encounter strong defenses, each move matched by a counter move, both players trying to outsmart the other, thinking ahead to possible contingencies and backup plans. Unfortunately, with billions of years of evolutionary tricks at its disposal, cancer is a grandmaster at the cell-survival game.
For example, in response to therapies that target specific gene alterations, cancer cells may, sometimes within days of treatment, start downregulating that gene. Researchers have documented this defense strategy in response to the chemotherapy drug doxorubicin, which somehow induced a more than twofold downregulation of its target, topoisomerase IIα.
Other known defense strategies include increased expression of drug efflux pumps that expel cancer drugs from the cell; increased expression of detoxification mechanisms; reduced susceptibility to apoptosis and other forms of cell death; increased ability to repair DNA damage; and a slowdown in cell division that alters the usual cell-death response to unrepairable DNA damage. And this is to say nothing of several other stratagems that occur outside the cell that help cancer dodge treatments.
Fortunately, advances in molecular profiling and biomarking can help oncologists to anticipate and overcome these moves. Currently, the number of molecular strategies varies among cancer types, and only a few molecularly targeted therapies exist for thyroid cancer. But last year saw an uptick in papers investigating thyroid cancer biomarkers, including these advances in molecular research that should help strengthen oncology’s Elo rating against this form of the disease.
Setting Up the Board: What is Thyroid Cancer?
The thyroid is a small, butterfly-shaped gland located in the neck that produces hormones controlling functions like heart rate and body temperature. The four main types of thyroid cancer are: papillary, follicular, medullary, and anaplastic. Thyroid cancer is relatively rare, accounting for only 2.2% of new cancers with an estimated 44,020 new cases and 2,170 deaths this year. Although it is a highly survivable cancer with a 98.4% five-year relative survival rate, the rare (2-3%) anaplastic form of the disease is one of the deadliest cancers, with a near 100% mortality.
Depending on the type of thyroid cancer, its stage, and individual attributes of the patient, treatment options may include surgery, radiation therapy, targeted therapy, watchful waiting, or a combination of these options.
Targeted therapy, the subject of this blog post, employs drugs to identify and attack cancer cells selectively, while largely sparing normal cells. For example, a class of drugs called tyrosine kinase inhibitors block signaling pathways that cancer cells need to grow. Another drug class, protein kinase inhibitors, inhibit the production of proteins needed for cell growth. These drugs are often used to treat anaplastic thyroid cancer in patients with certain mutations in the BRAF gene.
Developing the Pieces: What Biomarkers to Target?
Papillary thyroid cancer, which accounts for up to 90% of thyroid cancers, often begins as a suspicious looking thyroid nodule. However, abnormal yet benign nodules are difficult to differentiate from malignant tumors. Fine needle aspiration biopsies, the usual means of diagnosis, result in inconclusive findings about 30% of the time. Up to 75% of these patients undergo unnecessary surgeries to remove parts of the gland, according to a study presented at the American Association for Cancer Research (AACR) Annual Meeting 2024, held April 5-10.
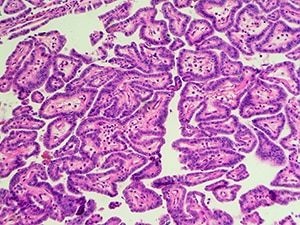
Because mutations in the BRAF gene are hallmarks of papillary thyroid cancer, the researchers wanted to see if identifying mutations in the biopsies would improve diagnosis. They used the qPCR technique with allele-specific probes to detect a BRAF V600E mutation in somatic DNA samples extracted from the biopsies of 99 patients. The mutation was detected in 28 of 50 patients who were later found to have malignant tumors and was detected in none of the 49 patients with benign tumors. Thus, the positive predictive value was 100%, and the negative predictive value 69.01%, working out to an accuracy of 77.78%, which led the researchers to conclude identifying the mutation could be a useful diagnostic tool.
The BRAF V600E mutation is also an important biomarker for anaplastic thyroid cancer, as it identifies patients who may be eligible for combination treatment with the protein kinase inhibitors, dabrafenib (Tafinlar) and trametinib (Mekinist). Another abstract presented at the AACR Annual Meeting concluded that a BRAF diagnostic test approved by the U.S. Food and Drug Administration (FDA) last year, the Oncomine Dx Target Test, was another valuable companion diagnostic for identifying these patients.
Middle Game, Battle Begins: Examining Treatment Strategies for thyroid cancer
This year, selpercatinib (Retevmo) an inhibitor of mutant forms of the RET tyrosine kinase, which is a protein that helps several cancer types grow, received approval from the FDA for certain advanced pediatric thyroid cancers in patients aged 2 or older. They include:
- Advanced or metastatic medullary thyroid cancer that requires systemic therapy and harbors a RET mutation.
- Advanced or metastatic thyroid cancer that requires systemic therapy, harbors a RET gene fusion, and is refractory to radioactive iodine.
- Locally advanced or metastatic solid tumors with RET gene fusion that have progressed during or after treatment with a systemic therapy or have no alternative treatment options.
Selpercatinib previously received approval for the same thyroid cancer indications in patients 12 and older in 2020 and for the same solid tumor indication in adults in 2022.
Because only a few multi-kinase inhibitors have been used to treat advanced thyroid cancer, there is a growing need to develop new drug targets. To this end, a paper published in Clinical Cancer Research investigated the molecular subtype-specific metabolic characteristics of thyroid cancers, with an eye toward identifying novel therapeutic targets.
Using a unique multi-omic analysis that combined metabolomics with transcriptomics by profiling freshly frozen thyroid cancer tissues, the study found increased activity in one-carbon metabolism in papillary thyroid cancer, follicular thyroid cancer, and especially anaplastic thyroid cancer. Additionally, follicular thyroid cancer cases with RAS mutations showed elevated branched-chain amino acid (BCAA) activities. The protein expression levels of the BCAA transporter (SLC7A5) and a key enzyme in one-carbon metabolism (SHMT2) increased in all the thyroid cancers, particularly in a subtype of anaplastic thyroid cancer that harbors multiple mutations and is highly aggressive, the study found.
Expression of SHMT2 plays a role in biosynthetic pathways and mitochondrial redox homeostasis, which supports cancer cell growth. And expression of SLC7A5 plays a role in cancer cell resistance by maintaining an essential intracellular amino acid pool. The study suggested both as possible future anticancer drug targets.
RAF kinase inhibitor drugs are effective against some cancers with BRAF mutations, but are limited by adaptive induction of ERK signaling, genetic alterations that induce BRAF dimerization, and poor brain penetration. In short-term assays in vitro, a new experimental brain-penetrating, pan-mutant BRAF inhibitor, which was developed to address these limitations, disrupted dimerization in BRAF V600E p61 splice variant melanoma cells. When researchers combined it with the MEK inhibitor binimetinib (Mektovi), it produced tumor regression in an in vivo model and significant, ongoing tumor regression (-80%) in a patient with BRAF V600E positive thyroid cancer.
These results were part of a first-in-human clinical trial published in Cancer Discovery which treated 30 patients with treatment-refractory BRAF solid tumors with the new drug in monotherapy and in combination with other drugs. When combined with binimetinib, the patients had an overall response rate of 57%, an improvement over exarafenib (17%) and plixoafenib combined with cobicistat (Tybost) (18%). Researchers suggested the new therapy might work by inhibiting RAF/MAPK signaling pathways in the tumor cells.
Endgame: Gaining a Tempo Post Progression
A BRAF fusion occurs when a BRAF gene joins with another gene. They are increasingly seen in standard multigene next-generation sequencing panels, but a paper published in Clinical Cancer Research highlights how few studies have explored their structure or their impact on cancer progression. In this study, researchers looked at fusion data from 69,337 cancer patients that were characterized and reviewed for oncogenic potential. They retroactively examined 241 BRAF fusion-positive tumors and found 82 unique fusion partners, 39 of which had never been reported on previously. These represent potential new therapy targets, researchers noted.
The study also found 15 patients whose tumors acquired BRAF fusions after receiving MAPK-directed therapies, and one of those was a papillary thyroid cancer patient. This finding underscores the importance of performing post-progression biopsies, the paper noted, citing a previous study in which patients who received targeted therapy after developing acquired resistance showed improved outcomes.
The oncology field continues to learn the deadly serious rules of molecular chess. But as the principles of drug resistance become clearer, there’s reason to hope for progress and better patient outcomes. After all, in the words of chess author Irving Chernev: “Every chess master was once a beginner.”