FDA Approvals in Oncology: July-September 2024
To help our readers keep track of the cancer therapies approved by the U.S. Food and Drug Administration (FDA), understand their impact for patients, and put them in context of the current therapeutic landscape, Cancer Research Catalyst provides a quarterly review of the latest approvals in oncology from the FDA.
From first-in-class therapeutics to expanded indications for standard-of-care drugs, the third quarter of 2024 brought some exciting treatment advances to the market.
This summer, the FDA issued a total of 16 oncology approvals spanning a range of therapeutic areas, including cell-based therapies, novel drug formulations, and broader eligibility for some immunotherapies. The approvals included five drugs that are new to the market, two of which are first in class.
New to the Market: Cells, Drugs, and a Tumor-seeking Toxin
The FDA had a particularly busy August in which they approved several brand-new therapeutics.
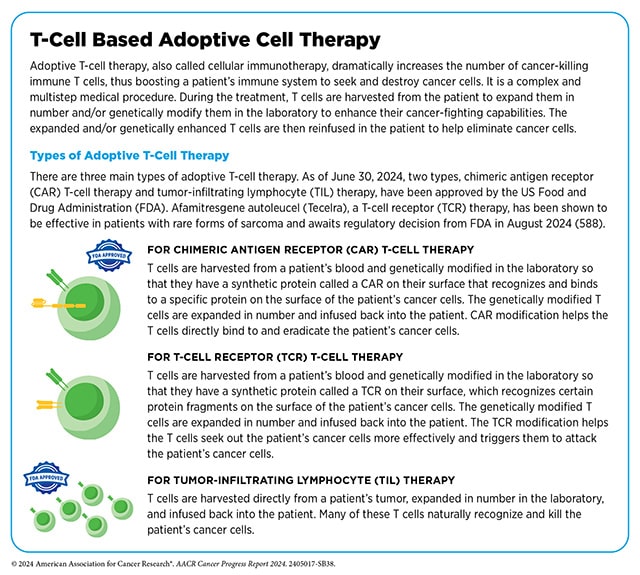
The first was a type of cellular immunotherapy called a T-cell receptor (TCR) T-cell therapy. Like chimeric antigen receptor (CAR) T cells, TCR T cells are made by harvesting T cells from the blood of cancer patients, engineering them in the lab to target cancer cells, and infusing them back into patients to fight cancer.
Unlike CAR T cells, TCR T cells are engineered to express a modified version of the naturally occurring T-cell receptor instead of a chimeric receptor. TCR T cells recognize tumor antigens presented by proteins called human leukocyte antigens (HLAs) whereas CAR T cells directly bind to target proteins on the surface of cancer cells.
- Afamitresgene autoleucel (Tecelra; afami-cel) is the first TCR T-cell therapy approved for use in cancer. It received accelerated approval this quarter for the treatment of certain adult patients with unresectable or metastatic synovial cell sarcoma, a type of soft tissue sarcoma, who have received prior chemotherapy.
Afami-cel is designed to recognize fragments of the protein MAGE-A4, which is expressed in some synovial cell sarcomas. It also recognizes the HLA proteins that present these fragments; because each individual has a different fingerprint of HLA types, afami-cel is approved to treat patients with MAGE-A4-positive tumors who test positive for an HLA recognized by afami-cel.
In addition to engineering living cells, researchers can also engineer specialized proteins that bring toxic molecules straight to cancer cells.
- Denileukin diftitox (Lymphir)—approved this quarter for patients with relapsed or treatment refractory cutaneous T-cell lymphoma—consists of the protein IL-2 bound to diphtheria toxin. The IL-2 portion of denileukin diftitox binds to the IL-2 receptor, which is strongly expressed on activated T cells, including malignant T cells. The drug is then brought inside of the cells, where the toxin is cleaved from IL-2 and poisons the tumor cells.
New drugs benefitted patients with a variety of other malignancies as well.
- Axatilimab-csfr (Niktimvo), an antibody that targets the protein CSF-1 on the surface of certain immune cells, was approved to treat chronic graft-versus-host disease (cGVHD), a serious side effect some patients develop after stem cell transplants used to treat certain hematologic malignancies. During cGVHD, immune cells arising from the transplanted cells recognize the patient’s healthy tissues as foreign and can attack them. Axatilimab-csfr suppresses the activity of monocytes and macrophages, which contribute to the widespread inflammation that can damage healthy tissues. Axatilimab-csfr is approved for patients whose cGVHD has not responded to at least two prior lines of therapy.
- The FDA approved the first targeted therapy for grade 2 astrocytoma or oligodendroglioma, two rare types of brain tumors that can occur in children and adults. Vorasidenib (Voranigo) inhibits mutant forms of the proteins IDH1 and IDH2, which can drive tumor growth. It is now approved for use after surgery in patients 12 years and older with grade 2 oligodendroglioma or astrocytoma harboring a susceptible IDH1 or IDH2 mutation.
One Target. Many Drugs.
This quarter, three therapies were approved to target the same driver mutations in non-small cell lung cancer (NSCLC).
Mutations in the epidermal growth factor receptor (EGFR) are common in NSCLC, especially in exons 19 through 21. The three EGFR-targeting therapies approved this quarter were all approved to treat patients whose NSCLC tumors harbor deletions in exon 19 or L858R mutations in exon 21.

- Lazertinib (Lazcluze) and amivantamab-vmjw (Rybrevant) were approved as a combination therapy for the first-line treatment of patients with locally advanced or metastatic disease. This was the first FDA approval for lazertinib, a small-molecule inhibitor of mutant EGFR. Amivantamab-vmjw is a bispecific antibody that also targets EGFR, but it additionally blocks the activity of MET, a receptor that can kickstart the same cell growth and proliferation processes.
- This quarter, amivantamab-vmjw was granted an additional approval in combination with chemotherapy for patients with locally advanced or metastatic NSCLC that had relapsed after treatment with another EGFR inhibitor.
- Osimertinib (Tagrisso), another small-molecule inhibitor of EGFR, was previously approved for the first-line treatment of patients with metastatic NSCLC and the adjuvant treatment of patients with resectable NSCLC with exon 19 deletions or L858R mutations. This quarter, it earned an approval to treat patients with stage 3 unresectable disease that did not progress during or after platinum-based chemotherapy.
What is Hyaluronidase? (And Other New Formulations)
This quarter’s approvals included two drugs formulated with the enzyme hyaluronidase, which breaks down hyaluronan, a component of the extracellular matrix. This can help drugs disperse more easily when injected under the skin and penetrate tumors to kill cancer cells.
- The formulation of atezolizumab and hyaluronidase-tqjs (Tecentriq Hybreza) was new to the market in September. Atezolizumab is an immune checkpoint inhibitor (ICI), an immunotherapy that blocks the immune system’s natural “brakes” to help immune cells fight cancer. While it is approved for many indications as an intravenous infusion, its formulation with hyaluronidase-tqjs is injected subcutaneously, a much faster delivery process.
While researchers were analyzing the efficacy of the subcutaneous formulation (which was comparable to that of the intravenous formulation for NSCLC), they also evaluated patients’ preference for one formulation over the other. Preliminary data showed that 70.7% of patients preferred atezolizumab and hyaluronidase-tqjs to the intravenous infusion. The current approval allows for atezolizumab and hyaluronidase-tqjs to be used in place of intravenous atezolizumab in all previously approved indications in adult patients. - The FDA approved a new indication for daratumumab and hyaluronidase-fihj (Darzalex Faspro), a subcutaneous formulation of the CD38-targeting antibody daratumumab first approved in May 2020 for certain patients with multiple myeloma. Since then, daratumumab and hyaluronidase-fihj has been approved for a total of seven multiple myeloma indications as a monotherapy or in various combinations.
The newest combination, approved in July, pairs daratumumab and hyaluronidase-fihj with the steroid dexamethasone, the immunomodulatory drug lenalidomide, and the protease inhibitor bortezomib for use in the induction and consolidation phases of therapy in patients with newly diagnosed multiple myeloma who are eligible for a stem cell transplant.
Bortezomib also received a separate approval as a new formulation.
- The new formulation of bortezomib (Boruzu) comes ready to inject, meaning it doesn’t need to be reconstituted by health care providers, and it can be used for all existing bortezomib indications for multiple myeloma and mantle cell lymphoma.
Bringing Treatments to Earlier Stages and Ages
Often, new drugs are first tested in patients with late-stage or treatment-refractory disease before being tested in earlier disease stages. This quarter, the indications for two drugs were expanded to include less advanced cancers.
- Durvalumab (Imfinzi)—an ICI that targets the immune checkpoint protein PD-L1, which is expressed on tumors and other cells—has previously only been approved for patients with advanced, metastatic, or treatment-refractory cancers. In August, the FDA greenlit durvalumab for the treatment of early-stage, resectable NSCLC. The approval allows durvalumab to be given with platinum chemotherapy in the neoadjuvant setting (before surgery) then as a single-agent adjuvant therapy (after surgery) to prevent recurrence. Results from the phase III AEGEAN trial, which led to the approval, were presented at the AACR Annual Meeting 2023.
- Isatuximab (Sarclisa) was approved for certain adult patients with newly diagnosed multiple myeloma. Like daratumumab, isatuximab is a CD38-targeting antibody that was approved for use in combination with bortezomib, lenalidomide, and dexamethasone. Unlike daratumumab, isatuximab was approved for patients who are not eligible for stem cell transplants.
Isatuximab has been approved in combination with other drugs for the treatment of relapsed or refractory multiple myeloma, but this is its first approval for newly diagnosed multiple myeloma. - Ribociclib (Kisqali), an inhibitor of the cyclin-dependent kinases 4 and 6, has been approved for use in patients with hormone receptor-positive, HER2-negative breast cancer since 2017, but only for patients with locally advanced or metastatic disease.
In September, the FDA approved ribociclib plus an aromatase inhibitor—a drug that blocks the production of estrogen from precursor hormones—for patients with stage 2 and 3 breast cancer with a high risk of recurrence after surgery. Results from the phase III NATALEE trial, which led to the approval, were presented at the 2023 San Antonio Breast Cancer Symposium. They simultaneously approved a co-pack consisting of ribociclib and the aromatase inhibitor letrozole (Femara) for the same indication.
Just as new therapies are typically tested in patients with advanced disease before those with early disease, they are also typically tested in adults before children. This quarter, one therapy that had previously been approved for adults and adolescents was approved for patients 2 years of age and older.
- Selpercatinib (Retevmo) received traditional approval for the treatment of adult and pediatric patients with advanced or metastatic medullary thyroid cancer (MTC) that harbors a mutation in the RET gene. Selpercatinib, a RET inhibitor, received an accelerated approval for this indication in May 2024 and has been approved since 2020 to treat patients with RET-mutated MTC who are 12 years and older.
Expanding Indications for Immune Checkpoint Inhibitors
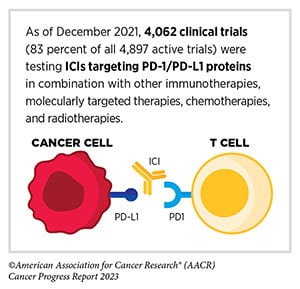
In the early days of ICI therapy, these drugs were primarily used to treat tumors that expressed certain checkpoint proteins. Eventually, researchers learned that some tumors were susceptible to ICIs in the absence of checkpoint protein expression. Molecular markers that may indicate strong expression of abnormal protein fragments—including mismatch repair deficiency (dMMR), high tumor mutational burden (TMB), and high microsatellite instability (MSI-H)—have been shown to also indicate susceptibility to ICIs. Therefore, several ICIs have been approved to treat tumors with dMMR, MSI-H, or high TMB regardless of checkpoint protein expression.
In recent years, researchers have found that some tumors without checkpoint protein expression respond to ICIs even in the absence of dMMR, MSI-H, and high TMB. This observation laid the groundwork for two new approvals this quarter.
- In September, pembrolizumab (Keytruda) plus chemotherapy was approved for the first-line treatment of patients with malignant pleural mesothelioma (MPM), a cancer of the chest cavity, with no biomarker requirements.
- Dostarlimab-gxly (Jemperli), an ICI targeting the same checkpoint pathway as pembrolizumab, also earned a biomarker-agnostic approval this quarter. In combination with the chemotherapies carboplatin and paclitaxel, dostarlimab-gxly is now approved for the treatment of adult patients with advanced or recurrent endometrial cancer. While it was approved in 2023 for such endometrial cancers characterized as dMMR or MSI-H, the current approval eliminates the biomarker requirements.
Check out our FDA approvals page for a comprehensive overview of each approval, including the clinical data that lead to each.


