Sexual Symptoms and Treatment Adherence After Breast Cancer
“It’s difficult for women to bring it up … You only have a small amount of time. So, you talk about other things.”
“I was like, ‘I don’t wanna take it.’ Everything in my body is saying don’t take this pill.”
Long before Janeane N. Anderson, PhD, MPH, began researching sexual symptoms following breast cancer treatment, she worked as a high school teacher in Texas.
“Abstinence-only was, and still is, the law of the land,” she recalled.
The culture of sexual silence in the U.S. South and the accompanying sexual health challenges eventually inspired her to become a researcher. As an assistant professor at the University of Tennessee Health Science Center, she’s found that the widespread discomfort of talking about sex extended into the clinic—even when it involves cancer care.
After surgery for early-stage, hormone receptor-positive breast cancer, patients are commonly prescribed a five- to 10-year regimen of adjuvant endocrine therapy (AET), a type of breast cancer treatment that helps to prevent recurrence by blocking the effects of estrogen. While it has proven quite effective in reducing the odds of recurrence in these patients, it can cause several side effects that many patients find hard to tolerate for up to a decade; in fact, over a third of patients discontinue their AET prematurely.
Anderson co-authored the 2023 study featuring the above quotes from women—specifically Black women—who received AET for early-stage breast cancer. But while the effects of AET on sexual health have been well documented anecdotally, comprehensive studies on their incidence and how they affect treatment adherence and survivorship remain lacking, Anderson explained.
At the 17th American Association for Cancer Research (AACR) Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved, held in Los Angeles, September 21-24, Anderson presented a study showing that Black and white patients experience sexual symptoms differently, and it impacts their lives and medication adherence in different ways.
Side Effects of Endocrine Therapy
Even after menopause, low levels of circulating estrogen help maintain musculoskeletal integrity, vascular function, and reproductive health. Eliminating the remaining estrogen via AET can cause symptoms similar to those seen during the transition to menopause, including hot flashes, night sweats, joint pain, mood swings, and vaginal dryness.
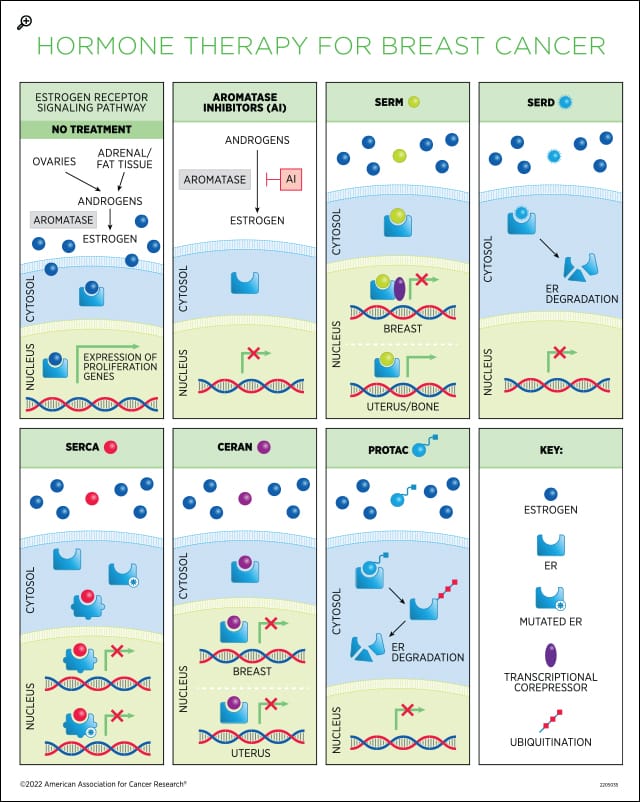
In a 2023 study published in the AACR journal Cancer Prevention Research, researchers analyzed the associations between common endocrine therapy symptoms and six-month adherence to treatment in patients treated in the NSABP B-35 phase III clinical trial. Patients in the trial were randomly assigned (1:1) to receive either anastrozole (Arimidex), an aromatase inhibitor that blocks the production of estrogen in postmenopausal women, or tamoxifen, a SERM that prevents estrogen receptor signaling in the breast but stimulates it in other tissues, including the bone and endometrium. This allowed the authors of the study to comprehensively characterize symptom burden and treatment adherence in patients receiving two different classes of endocrine therapy.
Symptoms significantly associated with time to treatment discontinuation for patients treated with anastrozole included body mass index (BMI), insomnia, joint pain, hot flashes, headaches, gynecologic symptoms, and vaginal discharge; for patients treated with tamoxifen, the symptoms included BMI, cognitive problems, joint pain, gynecologic symptoms, mood symptoms, weight problems, and pain with intercourse.
Researchers are now beginning to tease out which symptoms are most significantly associated with treatment adherence so they can more effectively monitor patients and intervene if necessary.
The problem, Anderson said, is that many existing studies don’t specifically address sexual symptoms for breast cancer patients. “Up to this point, we’ve mostly talked about AET symptoms as a collective,” she explained. “But in research interviews and informal conversations with more than 100 women over the last seven years, I’ve heard over and over that sexual health is one of the greatest unmet needs.”
Facing a Choice Between Quality of Life and Treatment Adherence
In their recently presented study, Anderson and colleagues sought to characterize the landscape of sexual health symptoms in 102 Black and 173 white patients receiving AET and how those symptoms affected both quality of life and treatment adherence.
Patients enrolled in the THRIVE clinical trial were surveyed at enrollment, six months, and 12 months about their symptoms, and their adherence was monitored via an electronic pillbox. Researchers used the 12-item Short Form Health Survey to monitor both physical and mental quality of life.

In a post-hoc analysis, vaginal itchiness, vaginal discharge, painful intercourse, and decreased libido were associated with lower mental quality of life in both Black and white patients at all three time points. However, loss of interest in sex was also associated with a lower physical quality of life in Black patients. Further, vaginal dryness (at six months), loss of interest in sex, and sexual satisfaction (at 12 months) were associated with lower AET adherence for Black patients but not for white patients.
Anderson emphasized that these findings not only demonstrate how bothersome these symptoms can be for women receiving AET but also that Black and white women experience them differently. Black women have a 40% higher risk of dying of breast cancer than white women, according to the AACR Cancer Disparities Progress Report 2024, and are more likely to skip or reduce prescribed AET doses that can prevent breast cancer recurrence.
Anderson feels strongly that acknowledging and addressing sexual symptoms in Black patients can help to close the mortality gap. “If we can start to address some of these symptoms, we may start seeing parity in Black and white women’s AET adherence,” Anderson said. “What that really means is that … families will get to keep their mother, sister, auntie longer.”
Fortunately, interventions exist to treat sexual health symptoms, Anderson explained. Vaginal moisturizers and topical estrogen may help with dryness, itching, and pain. Counseling can help boost a patient’s sexual self-image and facilitate conversations with their partner. Other hormonal therapies, including testosterone, are being evaluated as well.
But Anderson stressed that patient-centered communication is key to ensuring that patients understand their options and that such conversations should be initiated by the oncologist. In her team’s qualitative study featuring interviews with 32 Black women receiving AET for early-stage breast cancer, some women felt they would be seen as not taking their disease seriously if they expressed concern about their sexual symptoms.
Patients reported that they would be more comfortable discussing their sexual symptoms with a female provider and that peer support from fellow survivors—especially women of color—could help facilitate such conversations. Anderson hopes this information can help oncology practices create encouraging environments for Black women to share their experiences and receive the supportive care they deserve.
“With their cancer diagnosis, some women are making the decision to either reclaim some sense of their sexual self or to maintain [treatment] adherence,” Anderson said. “Hopefully, we can make it so that they don’t have to make that choice anymore.”