Neoadjuvant Immunotherapy for Liver Cancer: Shrinking Tumors, Growing Responses
In May 2022, Anibal Torres woke up with severe stomach pain that kept him from eating much over the next several days. He was eventually referred to the hospital for a CT scan that revealed a massive tumor in his liver—a hepatocellular carcinoma.
At 11.9 cm, it was too large to be surgically removed. A referral from Marcia Cruz-Correa, MD, PhD, the then-director of University of Puerto Rico Comprehensive Cancer Center, got him into a clinical trial testing an immunotherapy-based treatment regimen in patients with tumors like his. The hope was that the drug would shrink Torres’ cancer enough that it would be safe to operate.
Though he had some side effects, Torres gradually noticed improvements. “I’m eating better, I’m sleeping better, I’m doing everything better,” he said in the American Association for Cancer Research (AACR) Cancer Disparities Progress Report 2024, released in May. At the time, his tumor was down to 4.3 cm, and his doctors aimed to operate when it shrank below 4 cm.
Torres has since undergone a successful surgery and is doing well. His is just one success story among the many clinical trials currently evaluating neoadjuvant immunotherapy in liver cancer.
A recent study published in the AACR journal Cancer Research Communications analyzed patient outcomes from such trials and suggested that offering immunotherapy to patients with locally advanced tumors may improve their odds of a successful surgery.
Why Neoadjuvant Immunotherapy?
There are several reasons a locally advanced liver cancer may not be considered resectable, according to Mark Yarchoan, MD, an associate professor of oncology at the Johns Hopkins Kimmel Cancer Center and senior author of the study. The most common include multiple localized tumors, invasion into veins or arteries, or large tumors such as Torres’. Such high-risk features can present safety concerns and/or decrease the odds of a successful surgery.

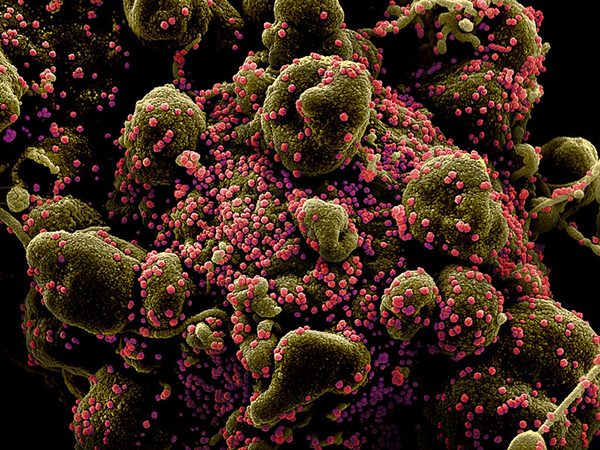
But neoadjuvant immunotherapy—immunotherapy given before surgery—can potentially shrink tumors so that they’re safer to remove.
Studies have shown another important advantage to neoadjuvant immunotherapy: Giving immunotherapy when the tumor is still intact provides the immune system with a bigger repertoire of antigens to mount a response against. This has translated to more robust immune responses when patients receive immunotherapy before surgery versus after.
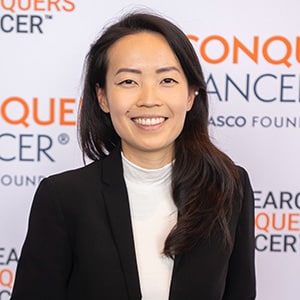
The benefits of this go even further, explained Mari Nakazawa, MD, a clinical research fellow at the Johns Hopkins Kimmel Cancer Center and first author of the study. A more activated immune system trained to recognize a broader library of antigens may be better poised to attack cells that have escaped the primary tumor to seed metastases elsewhere—so-called “micrometastases.” This may decrease the odds that the cancer will come back after a successful surgery.
“There’s a strong unmet need to expand the number of patients who may be eligible for surgery and, further, to transform more patients with early-stage liver cancer into long-term survivors of this disease,” Nakazawa said in a press release.
Does Neoadjuvant Immunotherapy for Liver Cancer have an Impact on Long-term Survival?
While other studies have shown that patients with unresectable liver cancer may respond well to neoadjuvant immunotherapy, Yarchoan, Nakazawa, and colleagues sought to characterize the long-term survival of such patients. They looked at outcomes from 92 patients who underwent curative resection—surgery intended to remove all evidence of disease—for hepatocellular carcinoma at Johns Hopkins. This included 46 patients who were treated with neoadjuvant immune checkpoint inhibitors (ICIs), most of whom were treated as part of clinical trials.
Importantly, 61.1% of these patients would not have been eligible for curative resection at intake based on existing eligibility criteria. Consistent with this observation, patients who received neoadjuvant ICIs more commonly exhibited high-risk features that typically predispose patients to worse outcomes.
Nevertheless, 94.4% of patients treated with neoadjuvant ICIs underwent a successful resection with negative margins. Yarchoan stressed that this was impressive in a group of patients for whom surgery would not have been advisable in the majority of cases.
In this study, however, patients who received neoadjuvant ICIs had comparable outcomes to those treated with surgery upfront. Patients who received neoadjuvant ICIs lived a median of 44.8 months without their cancer coming back, compared with 49.3 months among patients who did not receive neoadjuvant ICIs.
“This study shows that the criteria by which we classify patients as being candidates for curative therapy is probably too narrow for this disease,” Yarchoan said in a press release. “Systemic therapy may not only be useful for patients with advanced disease but can potentially be paradigm-changing in patients with early-stage disease.”
Yarchoan and Nakazawa stressed that the findings are retrospective, derived from a single institution, and compiled from several different clinical trials (or upfront surgery as the standard of care), and that further studies will be necessary to confirm. “Prospective trials that are thoughtfully designed in the right populations can help us understand which patients can benefit most from this approach,” Nakazawa said.
More clinical research in this area is certainly a notion patients like Torres can get behind. “We went through it. We’re living it. We’re seeing the results,” Torres said. “Thanks to all the research that’s coming out, I’m alive today, and I’m grateful.”