FDA Approvals in Oncology: October-December 2024
To help our readers keep track of the cancer therapies approved by the U.S. Food and Drug Administration (FDA), understand their impact for patients, and put them in context of the current therapeutic landscape, Cancer Research Catalyst provides a quarterly review of the latest approvals in oncology from the FDA.
The FDA had a busy 2024, issuing more than 60 oncology approvals, including for 11 first-in-class therapeutics. Approvals from January through September were discussed in previous blog posts:
- FDA Approvals in Oncology: January-March 2024
- FDA Approvals in Oncology: April-June 2024
- FDA Approvals in Oncology: July-September 2024
Here, we provide an overview of the 15 oncology approvals issued by the FDA during the final three months of 2024, which featured nine therapies new to the market, as well as some familiar drugs approved for new indications and as new formulations.
New Drugs, New Targets
Two new drugs against new targets were approved by the FDA this quarter for leukemia and gastric/gastroesophageal junction cancer. The approval of these drugs expands the number of molecular alterations that can be targeted for cancer treatment.
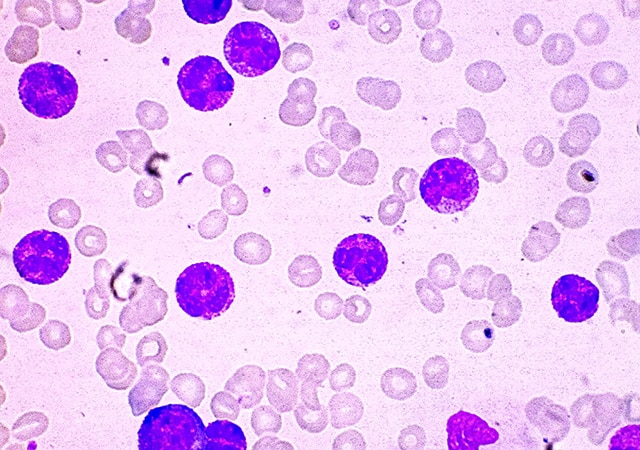
- Revumenib (Revuforj) was approved for the treatment of adult and pediatric patients 1 year and older with relapsed or treatment-refractory acute leukemia that harbors a translocation involving the lysine methyltransferase 2A (KMT2A) gene.
Revumenib inhibits a protein called menin, which works together with MLL1, the protein produced by the KMT2A gene, to regulate the expression of genes involved in hematopoiesis, among other processes. Translocations involving KMT2A are common in acute leukemias and can cause the MLL1/menin complex to turn on gene expression patterns that drive cancer. Revumenib blocks this process by preventing menin from interacting with MLL.
- The FDA also approved zolbetuximab (Vyloy) in combination with a chemotherapy regimen of fluoropyrimidine- and platinum-containing drugs for the first-line treatment of patients with locally advanced unresectable or metastatic gastric or gastroesophageal junction cancer whose tumors test positive for claudin 18.2 and negative for human epidermal growth factor receptor 2 (HER2).
Zolbetuximab is an antibody that targets the protein claudin 18.2, which is expressed at junctions between cells in the gastrointestinal tract and other organs. Cancer disrupts the normal architecture of cells and exposes claudin 18.2, leaving it vulnerable to therapeutic targeting. Zolbetuximab binds to claudin 18.2 and activates the immune system against claudin 18.2-expressing cells. Early clinical results evaluating zolbetuximab for gastric/gastroesophageal junction cancer were published in the American Association for Cancer Research (AACR) journal Clinical Cancer Research.
New Drugs, Old Targets
Also entering the market this quarter were six new drugs against familiar targets, such as PI3K proteins, CD19, HER2, PD-L1, and ALK. While other drugs targeting these proteins were previously available, the newly approved therapeutics offer potentially less toxic and longer-lasting alternatives.
A More Selective PI3K Inhibitor
Proteins within the PI3K family have been implicated in breast cancer, and preclinical data have shown that simultaneously targeting the interconnected PI3K, hormone receptor (HR), and CDK4/6 signaling pathways could enhance treatment efficacy and delay resistance. However, no such combinations had been FDA-approved because available PI3K inhibitors were too toxic once combined with these other therapies in the clinic, possibly because of their inhibition of multiple PI3K members. This quarter, the FDA approved the first regimen combining a PI3K inhibitor with HR-targeted and CDK4/6-targeted therapies for breast cancer treatment.
- The PI3K inhibitor inavolisib (Itovebi) was approved in combination with the CDK4/6 inhibitor palbociclib (Ibrance) and the hormone therapy fulvestrant (Faslodex) for patients with locally advanced or metastatic HR-positive, human epidermal growth factor receptor 2 (HER2)-negative breast cancer that harbors a mutation in the PIK3CA gene and has recurred on or after prior adjuvant endocrine therapy.
Unlike previously approved PI3K inhibitors, inavolisib is selective against mutant forms of the PI3K family member p110, which is encoded by PIK3CA and is mutated in about 35% to 40% of HR-positive breast cancers. This selective inhibition may make it less toxic and more tolerable when combined with palbociclib and fulvestrant compared with other PI3K inhibitors.
The molecular structure of inavolisib and its selective activity against p110 were first disclosed at the AACR Annual Meeting 2017, and the clinical trial results that led to inavolisib’s approval were reported at the 2023 San Antonio Breast Cancer Symposium (SABCS), which is co-organized by the AACR.
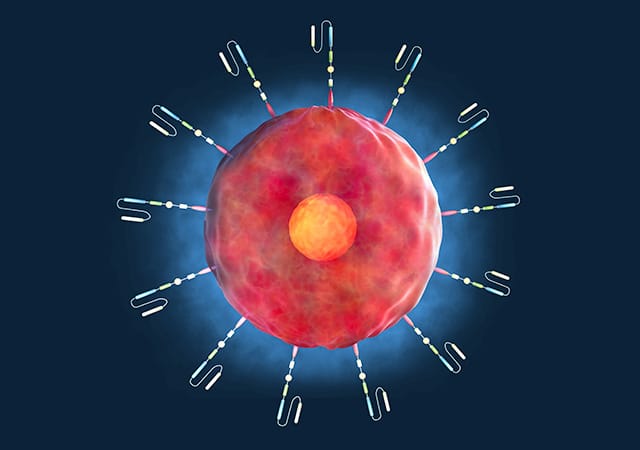
A Less Toxic CD19-directed CAR T Cell
Chimeric antigen receptor (CAR) T-cell therapy is a type of immunotherapy typically made from a patient’s own T cells. The T cells are extracted from the patient’s blood and engineered to target the cancer cells before being infused back into the patient. Multiple CAR T-cell therapies have been approved to treat leukemia and other hematologic cancers, but they can lead to severe immune toxicity. This quarter, the FDA approved a new CAR T-cell therapy with a unique design that may lead to fewer toxicities.
- Obecabtagene autoleucel (Aucatzyl) was approved to treat relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL).
Obecabtagene autoleucel is designed to target the CD19 protein that is often abundant on cancerous B cells, including in ALL. Obecabtagene autoleucel uses a different antibody fragment than previously approved CD19-directed CAR T-cell therapies to recognize CD19. The unique antibody fragment has lower affinity to CD19, which is predicted to help prevent severe toxic effects and improve T-cell expansion and persistence in the body.
Targeting HER2 With a Two-for-one Approach to Prevent Treatment Resistance
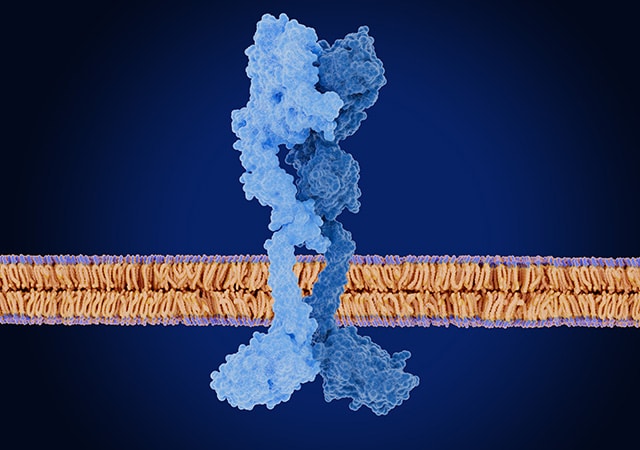
HER2 is a tumor-promoting protein overexpressed in many cancers. Several classes of HER2-targeted therapies are available, including for breast, gastric, and other HER2-positive cancers, but tumors frequently develop resistance to these treatments. This quarter, the FDA granted accelerated approval to two first-in-class therapeutics that use a novel strategy to help prevent resistance to HER2 inhibition: simultaneously binding two different targets.
- Zanidatamab (Ziihera) received accelerated approval to treat previously treated, unresectable or metastatic HER2-positive biliary tract cancer. Zanidatamab is a bispecific antibody that binds to HER2 in two different places, unlike most other HER2-targeting therapeutics that only bind to a single site. This double binding may help boost its efficacy compared to other HER2-targeting strategies approved for other cancer types.
Zanidatamab is the first HER2-targeting bispecific antibody approved for any cancer and the first HER2-targeting treatment for biliary tract cancer. Results from preclinical experiments with zanidatamab were published in the AACR journal Cancer Discovery. Zanidatamab is also being tested in a clinical trial for early-stage breast cancers, the results of which were presented at the 2023 SABCS.
- Zenocutuzumab (Bizengri) received accelerated approval for advanced, unresectable or metastatic non-small cell lung cancer (NSCLC) or pancreatic adenocarcinoma that harbors a gene fusion involving neuregulin (NRG1) and has progressed during or after prior systemic therapy.
Zenocutuzumab is a bispecific antibody that simultaneously binds HER2 and HER3 to prevent them from forming a complex with each other that can promote cell growth and drive resistance to other HER2-targeted therapies. Signaling through this complex is particularly high in cancers harboring NRG1 fusions due to NRG1-mediated activation of HER3.
Zenocutuzumab is the first HER2/HER3-targeting bispecific antibody and the first targeted therapy for tumors with NRG1 gene fusions to be approved by the FDA. Preclinical data showing the antitumor activity of zenocutuzumab, as well as early clinical data, were reported in the AACR journal Cancer Discovery. A presentation at the AACR Annual Meeting 2024 demonstrated that zenocutuzumab was effective in cancer models with high NRG1 expression.
The First PD-L1 Inhibitor for a Common Type of Skin Cancer
Cancer cells often hijack the PD-1/PD-L1 immune checkpoint pathway to suppress the antitumor immune response. Immune checkpoint inhibitors are immunotherapy agents that can counter immune suppression by blocking either PD-1 on immune cells or PD-L1 on cancer and other cells, allowing the immune system to attack cancer.
- This quarter, the FDA approved the PD-L1 inhibitor cosibelimab (Unloxcyt) to treat metastatic cutaneous squamous cell carcinoma (mCSCC) or locally advanced CSCC (laCSCC) not eligible for curative surgery or radiation.
CSCC is a type of skin cancer characterized by high mutation burden and upregulation of PD-L1. While PD-1 inhibitors have been approved to treat patients with mCSCC or laCSCC, cosibelimab is the first PD-L1 inhibitor to be approved for this patient population. Compared with PD-1 inhibition, PD-L1 inhibition has been shown to cause fewer high-grade immune-related adverse effects, and unlike some other immune checkpoint inhibitors, cosibelimab induces antibody-dependent cellular cytotoxicity, which may boost its efficacy. The preclinical characterization of cosibelimab was reported at the AACR Annual Meeting 2017.
A Second-generation ALK Inhibitor Adds to First-line Options
Anaplastic lymphoma kinase (ALK) is a protein that, when mutated, drives tumor growth in several cancer types, including NSCLC. Blocking ALK activity is a standard approach for treating newly diagnosed NSCLC, and many ALK inhibitors are available for this purpose, including a new one approved this quarter.
- Ensartinib (Ensacove) was approved to treat patients with ALK-positive locally advanced or metastatic NSCLC who have not yet been treated with an ALK inhibitor.
Ensartinib is a second-generation ALK inhibitor designed to overcome some of the challenges associated with the first-generation inhibitor crizotinib (Xalkori)—namely, the high rate of treatment resistance and low brain penetration.
Old Problem, New Strategy
Graft versus host disease (GvHD) is a common complication of the allogeneic stem cell transplants used to treat pediatric patients with blood cancers that develops when transplanted immune cells attack the patient’s healthy cells. Immune-suppressing steroids are the standard first-line treatment for patients who develop GvHD, but they are ineffective for many patients. While an inhibitor of the JAK signaling protein, ruxolitinib (Jakafi), was greenlit in 2019 for patients 12 years of age and older with steroid-refractory GvHD, it is not approved for younger patients.
- This quarter, the FDA approved remestemcel-L (Ryoncil), a therapy that delivers donor bone marrow-derived mesenchymal stromal cells, to treat children 2 months of age and older with acute GvHD that does not respond to steroids.
In addition to being the first FDA-approved therapy for steroid-refractory GvHD in patients younger than 12, remestemcel-L is also the first FDA-approved therapy to use mesenchymal stromal cells to suppress immune activity.
Old(er) Drugs, New Indications and Formulations
Sometimes, what’s old is new again, and this quarter, the FDA seemed to agree. Several previously approved drugs, including one that has been on the market for more than three decades, were greenlit for new indications.
Updated Labeling for a Chemotherapy Drug
- The FDA approved updated labeling for fludarabine phosphate, a chemotherapy drug first approved in 1991. The updated labeling includes new and revised indications that allow fludarabine phosphate to be used as a component of a combination regimen for the treatment of B-cell chronic lymphocytic leukemia (CLL) and as monotherapy for CLL that is refractory or that progressed during prior treatment with at least one alkylating agent-containing regimen.
These approvals occurred under Project Renewal, an initiative of the FDA Oncology Center of Excellence aimed at reviewing real-world data to update the approved indications for older drugs. AACR has worked with the FDA Oncology Center of Excellence to advance Project Renewal, providing scientific advice and perspective.
New Indications and a New Formulation for Immune Checkpoint Inhibitors
- Durvalumab (Imfinzi), first approved in 2017, was approved in December for adults with limited-stage small cell lung cancer (LS-SCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy. This approval makes durvalumab the first immunotherapy approved for patients with LS-SCLC. Durvalumab has been approved for several other types of cancer, including a more advanced form of SCLC known as extensive-stage SCLC.
- Neoadjuvant nivolumab (Opdivo) was approved in combination with platinum-containing chemotherapy, followed by adjuvant nivolumab alone, for patients with NSCLC that can be surgically removed, is 4 cm or larger or has spread to the lymph nodes, and is not known to harbor mutations in the epidermal growth factor receptor (EGFR) gene or rearrangements involving the ALK gene.
Since its first approval 10 years ago, nivolumab has been approved to treat several types of cancer, including NSCLC. Prior to this approval, it had been approved to treat some resectable NSCLC tumors in the neoadjuvant setting; the latest approval allows it to be used in the adjuvant setting as well.
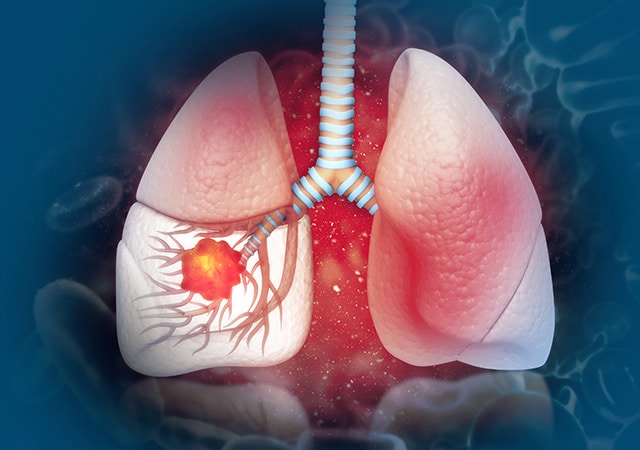
- The FDA also greenlit a new formulation of nivolumab that can be delivered by subcutaneous injection instead of intravenous infusion. Nivolumab and hyaluronidase (Opdivo Qvantig) was approved for subcutaneous injection in adults across approved solid tumor nivolumab indications as monotherapy, maintenance therapy, or combination therapy.
New First-line Indications for Targeted Therapy Drugs
- Encorafenib (Braftovi) was granted accelerated approval in combination with the EGFR inhibitor cetuximab (Erbitux) and the chemotherapy regimen mFOLFOX6 for patients with metastatic colorectal cancer harboring a BRAF V600E mutation.
Encorafenib, first approved in 2018, inhibits the tumor-promoting activity of mutant BRAF. Cancer cells can become resistant to BRAF inhibitors by upregulating EGFR activity; therefore, combining encorafenib with the EGFR inhibitor cetuximab may help prevent this resistance mechanism.
The combination of encorafenib and cetuximab was previously approved for patients with metastatic colorectal cancer who had already undergone previous treatments. The current approval establishes encorafenib, cetuximab, and mFOLFOX6 as an option for the first-line treatment of these patients. The preclinical efficacy of this regimen was demonstrated in a study published in the AACR journal Clinical Cancer Research.
- Asciminib (Scemblix), first approved in 2021, was granted accelerated approval this quarter for adults with newly diagnosed, Philadelphia chromosome (Ph)-positive chronic myeloid leukemia (CML) in chronic phase. The drug inhibits the tumor-promoting activity of the BCR-ABL fusion protein that is produced by an aberrant DNA fragment known as Ph. While other BCR-ABL-targeted drugs are approved for first-line treatment of CML, asciminib targets a different region of the protein that may help bypass treatment resistance.
Asciminib has been approved for certain patients with CML who have received prior BCR-ABL-targeted treatment as well as for patients whose CML harbors a mutation in BCR-ABL that makes it resistant to other therapeutics. The latest approval makes asciminib available to patients who have not yet undergone treatment for the disease, whether or not their cancer has the resistance-conferring mutation.
Check out our FDA approvals page for a comprehensive overview of each oncology approval, including the clinical data that lead to each.



