Experts Forecast Cancer Research and Treatment Advances in 2025
Every new year brings excitement and anticipation for what might happen over the next 12 months. So, what’s in store for 2025 that could change the way we diagnose and treat cancer? What first-in-class therapeutics could offer new life-saving options to patients? What scientific discovery will have everyone talking?
In 2024, we saw the approval of oncology drugs for more than 50 indications, including 11 first-in-class therapeutics. One of those—the first tumor-infiltrating lymphocyte (TIL) cell therapy—involved research dating back over 30 years. That only illustrates the time and dedication sometimes required to take breakthroughs from bench to bedside, making predictions challenging. Thought leaders in oncology, however, have their finger on the pulse of the field, as witnessed though our annual Experts Forecast series.
This year, we spoke with five leaders about the advancements they are most looking forward to in their respective fields:
- Precision Medicine – AACR President-Elect Lillian L. Siu, MD, FAACR;
- Immunotherapy – Vinod P. Balachandran, MD;
- Hematologic Malignancies – AACR Hematologic Malignancies Working Group Steering Committee Member John E. Dick, PhD, FAACR;
- Artificial Intelligence – Regina Barzilay, PhD; and
- Cancer Disparities and Prevention – Scarlett Lin Gomez, PhD, MPH.
Advances in Precision Medicine in 2025
Siu, director of the Phase I Clinical Trials Program, BMO Chair in Precision Cancer Genomics, and codirector of the Bras and Family Drug Development Program at the Princess Margaret Cancer Centre, University Health Network, believes we are about to enter a new era for drugging the undruggable with the next generation of mutant-specific molecules. She explained how the RAS space is still very active as we move beyond the first-generation KRASG12C inhibitors—sotorasib (Lumakras) and adagrasib (Krazati)—to second-generation inhibitors of this variant as well as early phase I evaluation into KRASG12D, KRASG12V, pan-KRAS, and pan-RAS inhibitors. In addition to small molecule inhibitors, therapeutic cancer vaccines and T-cell receptors are other modalities actively targeting this oncogene.
“These variants and mutations are common across multiple tumor types,” Siu explained. “We could see very exciting data in the next year or so with these types of novel RAS-specific inhibitors in tumors that were previously deemed very difficult to target using a precision medicine approach, such as pancreatic cancer.”
Siu also sees advances in technologies such as spatial transcriptomics, single-cell sequencing, and artificial intelligence (AI) and machine learning (ML) helping to further our understanding of the tumor microenvironment, which could result in more effective targeted therapies and immunotherapies. For example, she suggested that using AI/ML to analyze hematoxylin and eosin (H&E) slides and impute transcriptomic profiles of a patient’s tumor sample may spot hints of treatment response or resistance earlier than currently available methods. This could be particularly beneficial for immunotherapies where identifying predictive biomarkers has been challenging, Siu said.
“Other than PD-L1, microsatellite instability (MSI) status, and tumor mutational burden, there aren’t really any validated biomarkers for immunotherapy selection,” she explained. “But with high-resolution spatial technologies and perhaps the implementation of AI/ML in digital pathology, we may have a higher chance of identifying additional predictive biomarkers as well as novel immunotherapy targets or combinations that would be more effective than current strategies.”
Another method for monitoring response to treatment that researchers have been examining is the detection of circulating tumor DNA (ctDNA). In the coming year, Siu expects to see more early-phase clinical trials incorporate ctDNA testing to guide dose escalation and optimization and perhaps even aid in making go/no-go decisions about whether a trial should move forward to a later phase. However, she stressed that while ctDNA may be helpful as a short-term biomarker in clinical trials, it is not sufficient to use as the only endpoint at the present time.
“We have to follow patients through to see whether that clearance of ctDNA could actually predict and correlate with long-term outcomes, such as event-free survival and overall survival,” Siu explained.
Another trend she thinks will continue in 2025 is the increased focus on clinical trials for neoadjuvant therapies, especially ones that are built around immunotherapies or targeted treatments that have already shown positive results in other cancer types.
“We will continue to see drugs moving into earlier disease treatment settings, because this is where we would make the biggest difference in increasing cancer cures,” Siu said.
This could include advancements in cancer vaccines and antibody-drug conjugates (ADCs), two other drug classes Siu said she will be watching closely in 2025. In terms of therapeutic cancer vaccines, she will keep an eye on the ongoing clinical trials for neoantigen vaccines in patients who have very low tumor burden, such as those with molecular residual disease. While for ADCs, she is interested in following the progress with identifying biomarkers for ADC selection beyond immunohistochemistry, such as by looking at the cytoplasmic and membrane ratio of the expression of specific targets, as well as the progress with novel ADC designs.
“Just as important as the target is the linker and the payload,” Siu explained. “A lot of the toxicity for ADCs stems from the payload because they tend to cause myelosuppression, neuropathy, etc., so there is an urgency in the field to find payloads that have higher therapeutic index without causing as much toxicity.”
Advances in Immunotherapy in 2025
In the immunotherapy realm, Balachandran is also excited to track the progress of ADCs as one of several methods for harnessing immune recognition to fight cancer that he believes will advance in 2025.
“The ability to target tumor proteins with an ADC—an antibody attached to a toxic payload—really opens up the opportunity to test a variety of different targets for a variety of different indications,” he explained. “In 2025, I’ll be watching for the discovery of novel targets for ADCs as well as application of existing targets to new cancer types.”
As director of The Olayan Center for Cancer Vaccines at Memorial Sloan Kettering Cancer Center, Balachandran will also be closely watching the expanding research into cancer vaccines. He said that there has already been early proof of concept that vaccines may help the immune system fight cancers that typically harbor very few mutations, such as pancreatic cancer and glioblastoma, as well as highly mutated cancers like melanoma.
“It’s still early, but excitingly, there are now many ongoing clinical trials testing vaccines against mutation-derived antigens in cancers that span the mutational spectrum,” Balachandran said. “The results of these trials will provide us with a better understanding of what cancers might be best suited for treatment with a vaccine.”
Most of these ongoing efforts are in the adjuvant space, Balachandran explained, where the cancer vaccine is being used for secondary prevention after the primary cancer has been removed, with the goal of interrupting the cancer from returning. There are also efforts to examine cancer vaccines as primary prevention, but Balachandran does not expect such trials to report results in 2025.
“Cancer vaccines for primary prevention are mainly focused on scenarios where there is a higher inherent chance of cancer forming, such as with Lynch syndrome where tumors develop as a consequence of deficiencies in the mismatch repair pathway,” he explained. “Clinical trials in this space will be very interesting, but it will take a longer time for us to understand the results.”
Another question that Balachandran is interested to see addressed in the coming years is whether cancer vaccines must be personalized for one or more antigens based on a patient’s tumor or if off-the-shelf vaccines for shared antigens common among multiple patients would be just as effective.
“We do not know whether a specific antigen class is superior or not when targeted with a vaccine, so it will be important to look at the science. The data that emanate from these trials will help us understand if both ways might work or if one is better,” he said.
A similar query is being explored regarding cell-based therapies like chimeric antigen receptor (CAR) T-cell therapy. Most CAR T-cell therapies use autologous T cells, meaning they are extracted from a patient, re-engineered to recognize and attack cancer cells, and then infused back into the same patient. This process, however, requires expertise, and is time consuming and cost prohibitive, limiting scalability. But allogeneic CAR T-cell therapies are currently being tested to see if an off-the-shelf version could be developed that uses T cells from healthy donors.
“The field is realizing that scalability is crucial to increase access, so it will be important to see if off-the-shelf approaches that simplify the process are feasible,” Balachandran explained.
In the shorter term, Balachandran will be monitoring the expansion of cell-based immunotherapies to treat more cancer types following the first FDA-approved TIL therapy to treat metastatic melanoma—making it the first cell-based immunotherapy approved for a solid tumor. He also sees research into cancer vaccines and cell-based therapies as interconnected in ways beyond the question of off-the-shelf options, as both approaches fundamentally rely on the interaction between immune cells and cancer antigens.
“It’ll be exciting to see how information we gather from one method impacts the other and vice versa,” Balachandran said.
Advances in Hematologic Malignancies in 2025
Dick, a senior scientist at the Princess Margaret Cancer Centre, also foresees progress being made with allogeneic CAR T-cell therapies becoming more widely accessible in the near future. That is just one of his predictions related to how advances in immunotherapies will have an impact in treating hematologic malignancies.
“In blood cancers, one of the issues is that in some ways the easy things have been done, and now it’s time to tackle the more challenging problems,” explained Dick. “We have advanced therapies that can target the vast majority of the cells of a tumor based on defined phenotypes and genetic driver profiles, but there are two problems: tumors can possess rare drug tolerant cancer cells and cancer stem cells that drive recurrence; and therapies can also kill noncancerous cells. Now the challenge is to develop treatments that are more selective for targeting all classes of cancer cells present in the tumor. We are seeing advances in trying to find a more combinatorial T-cell targeting therapy where you can target a cancer-specific marker including cancer stem cells while leaving normal cells alone.”
For example, Dick is most excited by the idea of developing CAR T cells that are coded by a sort of a Boolean logic. In these cases, the CAR T-cell therapy would have multiple receptors with at least two different targets that are known to be associated with leukemia. The therapy only activates when it finds a cell with both leukemia markers, helping to spare healthy cells.
Dick said researchers are also exploring other ways to spare healthy cells when treating patients with blood cancers. This includes bispecific antibodies that only target the tumor and then bring in cells of the immune system to kill the cancer cells.
Like Siu, Dick is also intrigued by the latest research into understanding how some cancer cells are able to resist treatment and eventually even regrow the tumor.
“There’s increasing evidence that along the evolutionary process of some hematologic tumors that certain cells are fated to resist therapy,” Dick explained. “These cells are already there the day the person walks into the clinic. They can be very rare elements of the tumor, but they are already wired with metabolic and epigenetic properties that cause them to resist standard therapy.”
According to Dick, advances in single-cell analysis of gene expression, chromatin accessibility, and methylation are helping to identify these cells and offer a better understanding behind the wiring that keeps them in the state of being able to both resist therapy and later regenerate a recurrence. Dick also pointed to how these technologies are offering a wider look at the genome, which is unlocking additional information about resistance to treatments.
“Cancer isn’t just a disease of genes that have gone bad; 98% of the genome contains noncoding regions with very important cancer-specific regulators,” Dick explained. “There is a lot of cancer-related information in these regulatory regions, and we are finding that the reason some cancer cells resist therapy is often not a genetic lesion or a mutation, but a change in cell state influenced by these noncoding regions and other epigenetic processes.”
Dick’s own previous work in identifying stemness properties in leukemia cell states helped find predictors of treatment response, but he believes our understanding of cell states will advance further in 2025. This includes a deeper understanding of clonal hematopoiesis, a natural feature of aging in which one blood stem cell can pick up a clonal advantage over many other stem cells. In cases of TET2-mediated clonal hematopoiesis of indeterminate potential (CHIP), these mutated CHIP stem cells are the first step in the evolution towards leukemia and the cell of origin, leading to an increased risk for hematological malignancies. They also contribute to unrelated diseases including cardiovascular disease and even influence treatment responses for solid tumors.
“It’s become clear that clonal hematopoiesis is influencing how immune checkpoint inhibitor therapy works in certain subsets of patients,” Dick said. “We already know that there’s often crosstalk between a solid tumor and the blood system or the immune system, but now there is work that implicates clonal hematopoiesis as another factor that has been previously unrecognized. This is a going to become a major player in how patients with any kind of solid tumor will respond to therapy.”
It could also play a role in a new era Dick sees us entering in which we are able to target cancers much earlier in their evolution. He said the insights we gather about clonal hematopoiesis and by monitoring cell-free DNA and methylation signatures could allow us to target cancers in a premalignant state.
“There’s been a huge advance in the ability to map the cell of origin for a blood malignancy,” Dick explained. “If we can find these premalignant cells to target them, we can prevent them from progressing to cancer.”
Advances in Artificial Intelligence in 2025
Predicting future risk of cancer is at the center of much of Barzilay’s work. The health AI faculty lead of the Jameel Clinic at the Massachusetts Institute of Technology has been collaborating on projects that use AI to predict lung cancer and breast cancer years before diagnosis.
“We’ve seen some really exciting results in which the performance of machines rivals the performance of human experts,” Barzilay said. “Not only that, but AI models can actually give us reliable trajectories of future cancer development.”
This could have two implications in the years ahead, according to Barzilay. One, it would indicate which individuals may want to get screened more frequently. Two, which Barzilay said is even more exciting, it would help identify potential participants for chemotherapy prevention trials, which could lead to new therapeutics designed to prevent cancer but have so far been difficult to conduct without knowing who is likely to develop the disease.
“Until very recently, most of the AI research really focused on radiology and pathology, which are extremely important, of course, but they definitely do not cover everything in cancer research and care,” Barzilay explained. “Now there’s a lot of excitement related to molecular modeling, like AlphaFold, and new avenues for research that are building on the experimental data that has been collected for decades.”
For example, the Chan Zuckerberg Initiative, which helps to build open-sourced software that leverages AI to advance biomedicine research, has continued to release resources from the global Human Cell Atlas and other projects that are allowing researchers to build models that can characterize cell states and behaviors. Additionally, large amounts of biomolecular patient data are becoming available from blood analysis, imaging, cell sequencing, and more.
“Typically, you specialize in a particular field and have access to just one of these data sources, but I think we are moving towards the multimodal analysis of all of these data, which could give us very powerful tools to rethink the diagnosis and treatment of cancer,” Barzilay said.
One program she will be watching closely is ADAPT from ARPA-H, which will track tumor changes through multiple lines of therapy in patients and offer a central hub where clinicians and researchers can access that data. The goal is to use that information to predict which mutation a cancer will develop to escape the current line of treatment and perhaps offer a personalized plan for what treatment to give a patient next.
While this project is still ongoing, Barzilay said we already have AI tools ready to be used in the clinic—but the health care infrastructure is not set up for them. She pointed out that cancer screening guidelines from the National Comprehensive Cancer Network (NCCN) and United States Preventive Services Taskforce (USPSTF) have limited recommendations for using AI. Additionally, researchers found that coverage of AI-based tools by insurance companies in the United States is lacking, so using such tools could lead to financial toxicity for patients. Current regulatory guidelines are also not supportive of rapid changes happening in AI, according to Barzilay, who added regulators need to have a better understanding of what is safe and secure for patients.
“I hope that 2025 will be the year where it changes and we are putting our efforts as clinicians, researchers, and even as patients together and are lobbying the use of AI technology in health care,” she said. “We really need to recognize the opportunity AI provides—we cannot continue with the status quo because it costs lives and causes suffering.”
AI researchers can also do their part by involving clinicians more directly in the implementation of programs within the clinic, the design of trials, and even the design of the tools. Barzilay said it is crucial to get the clinical community engaged, so they can better understand how the programs work and would be more willing to use them.
As for the issue of bias in AI technology, Barzilay explained that while this is a serious problem, AI could potentially be part of the solution.
“By doing very large-scale testing on a diverse population, we can really address the issue of bias and help to better provide equitable care for the whole population,” Barzilay said.
Advances in Addressing Cancer Disparities and Prevention in 2025
As an epidemiologist, Gomez sees the advantages AI can bring when analyzing complex multidimensional data to better understand issues around cancer health inequity. But she said we also must tread carefully when implementing this technology.
“As the data scientists are developing AI algorithms, we need to be sure they’re working hand-in-hand with disparities researchers, epidemiologists, and community members to ensure we are not further exacerbating disparities through the development of these algorithms,” explained the coleader of the Cancer Control Program at the University of California, San Francisco (UCSF) Helen Diller Family Comprehensive Cancer Center. “But there is a lot of potential to rapidly accelerate discoveries regarding what factors are contributing to disparities, the intersections of those factors, and how that may potentially inform interventions.”
Emphasizing that cancer disparities are the result of multiple factors, Gomez said the focus in 2025 is on recognizing the upstream factors that lead to cancer. These are the structural and social drivers of health, including structural racism and the neighborhood conditions by which people live, work, play, grow, and pray.
“Unless we focus on these most upstream factors, we’re not going to fully eliminate cancer health disparities,” said Gomez, who was awarded the 2024 AACR Distinguished Lectureship on the Science of Cancer Health Disparities. “I already see some substantial efforts moving in that direction, including studies that are focusing on developing different measures of structural racism and the effects of policies on mediating cancer outcomes.”
An area that Gomez and her team will be looking at more closely in 2025 is the concept of ethnic enclaves, which have traditionally been defined as neighborhoods with a higher concentration of specific groups. In previous research, they have found that Asian Americans living in ethnic enclaves tend to have better survival outcomes than their counterparts, while Hispanics living in Hispanic enclaves tend to have worse cancer outcomes. Now, they want to understand what makes each ethnic enclave different.
“By trying to further differentiate ethnic enclaves and clarify the specific attributes of a place, we can pinpoint some of the protective but also potentially deleterious factors,” Gomez explained.
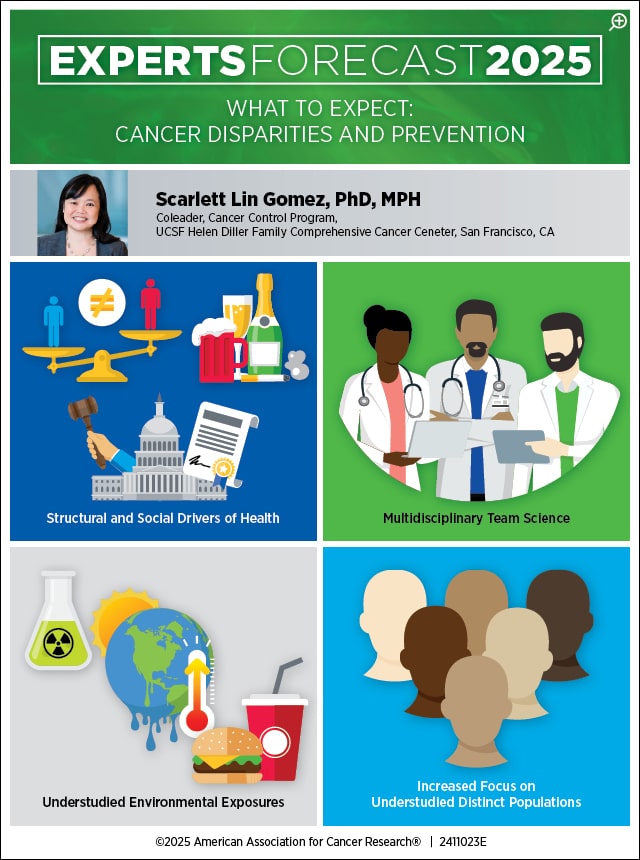
In 2025, Gomez can also see more research being done on previously understudied exposures that promote cancer, such as climate change. The effects of climate change have been found to disproportionately impact those in socioeconomically deprived areas, including during heat waves where urban areas create “heat islands” and are more likely to lose power.
“Populations that are already more at risk of adverse cancer outcomes are going to be further disadvantaged due to climate impacts,” Gomez said. “Hopefully research into climate-induced disparities can also help to motivate policy changes to mitigate some of the impacts of climate change.”
Gomez also expects disparities researchers to devote more attention to populations that have traditionally not been studied as much. For Gomez, this involves zeroing in on some of the distinct populations that generally get lumped together under the broad category Asian American, Native Hawaiian, and Pacific Islander as well as the various ethnicities that are often boiled down to just Hispanic. Beyond her own work, she is also excited by some of the initiatives that are attempting to collect more data from cancer patients of various sexual orientation and gender identity.
“Even as we are studying these distinct populations, we are moving away from looking at social identities as independent factors,” Gomez explained. “We know that it’s not just about being of one particular racial and ethnic group. It’s not just about living in a rural versus urban area. It’s not just about identifying as female versus male. It’s about the intersection of all of these characteristics together. So, I’m hopeful we will start to see more methods looking at intersectionality across social identities.”
Pulling this off will require large initiatives involving multidisciplinary teams. Gomez said this idea of team science has been much discussed over the past decade but has been difficult to actually achieve.
“We’re all trained in our very specific disciplines, and coming together to tackle one problem while critically thinking about how these different disciplines intersect is in reality very challenging,” Gomez explained. “But I feel like we’re finally starting to see that come to fruition to help to facilitate cells-to-society research.”



