A New Treatment Option for HER2-Positive Breast Cancer
The FDA has approved a new molecularly targeted therapeutic for treating certain patients with advanced or metastatic HER2-positive breast cancer.
The U.S. Food and Drug Administration (FDA) has approved a new HER2-targeted therapeutic called tucatinib (Tukysa) for treating patients who have advanced or metastatic HER2-positive breast cancer that has progressed despite treatment with one or more other HER2-targeted therapeutics.
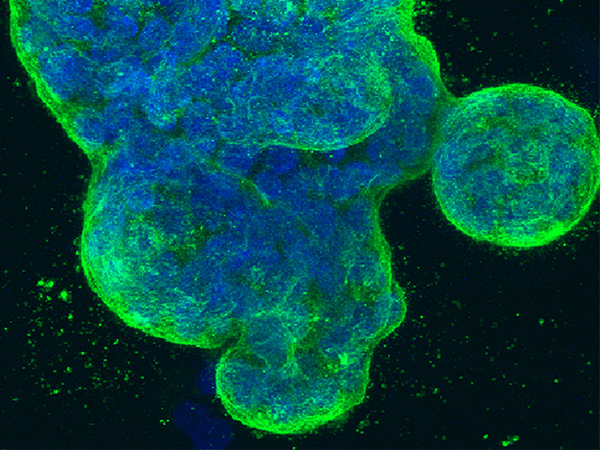
About 15 percent of the 276,480 new cases of breast cancer expected to be diagnosed in the United States in 2020 will have elevated levels of the protein HER2. HER2-positive breast cancer tends to be aggressive, and the outcome for patients was typically poor until research led to the development and FDA approval of HER2-targeted therapeutics. Trastuzumab (Herceptin) was the first of these groundbreaking therapeutics to be approved by the FDA, in 1998.
There are now numerous HER2-targeted therapeutics approved for treating advanced or metastatic HER2-positive breast cancer. Most patients are first treated with a combination of trastuzumab, a second HER2-targeted therapeutic called pertuzumab (Perjeta), and a cytotoxic chemotherapeutic. Despite the success of this combination, many patients ultimately have disease progression and new options for treating these individuals are urgently needed.
Tucatinib is a new HER2-targeted therapeutic. It has been approved by the FDA for use in combination with trastuzumab and the cytotoxic chemotherapeutic capecitabine.
The approval of tucatinib was based on results from the randomized, placebo-controlled phase II HER2CLIMB clinical trial, which were published in The New England Journal of Medicine and presented at the San Antonio Breast Cancer Symposium in December 2019. Among the first 320 patients who received tucatinib, trastuzumab, and capecitabine, the median time to disease progression was 7.8 months, compared with 5.6 months among the 160 patients who received placebo, trastuzumab, and capecitabine.
Further analysis took place after more patients enrolled in the trial, and it was found that tucatinib significantly improved overall survival. Among the 410 patients who received the tucatinib combination, the median overall survival was 21.9 months, compared with 17.4 months among the 202 patients who received the placebo combination.
Of interest, tucatinib significantly improved progression-free survival for patients who had metastases in the brain, which are particularly hard –to treat. Among the patients with brain metastases, 25 percent of those who received the tucatinib combination had not had disease progression at one year, compared with 0 percent of those who received the placebo combination.
The Australian, Canadian, Singaporean, and Swiss regulatory agencies approved tucatinib at the same time as the FDA as a result of a recently launched FDA initiative called Project Orbis to increase collaboration among different countries. This is the first time that the FDA has collaborated with the Singaporean and Swiss regulatory agencies in this way, but it has previously collaborated with the Australian and Canadian regulatory agencies on Project Orbis. The FDA hopes that further collaborations through this initiative will help patients with cancer around the world to receive earlier access to groundbreaking new treatments.
The FDA approval was rendered on April 17, 2020.
