Antibody-drug Conjugate for Acute Lymphoblastic Leukemia Approved for Pediatric Use
The FDA has approved inotuzumab ozogamicin for pediatric patients with certain leukemias.
The U.S. Food and Drug Administration (FDA) has approved inotuzumab ozogamicin (Besponsa) for the treatment of pediatric patients aged 1 year or older with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL) that expresses the protein CD22.
Inotuzumab ozogamicin is an antibody-drug conjugate, a type of therapy that consists of a toxic drug and an antibody that directs the drug to target cells. Inotuzumab, the antibody portion of inotuzumab ozogamicin, targets CD22 on blood cells called B cells that grow out of control in some types of ALL. Ozogamicin, the toxic drug portion of inotuzumab ozogamicin, damages DNA and leads to cell death.
Inotuzumab ozogamicin was approved by the FDA in 2017 to treat adult patients with CD22-positive B-cell precursor ALL that did not respond to or relapsed following other therapies. The current approval expands the indication to include children 1 year of age or older.
This approval was based on results from a multicenter, single-arm, open-label, phase II clinical trial that recruited 53 patients between the ages of 1 and 22 with relapsed or refractory CD22-positive B-cell precursor ALL. Patients received one of two dose levels of inotuzumab ozogamicin after treatment with methylprednisolone, an antihistamine, and a fever reducer to mitigate side effects.
Forty-two percent of patients experienced a complete response, with a median duration of 8.2 months. The vast majority of patients who experienced a complete response had no evidence of minimal residual disease (MRD, trace indicators of leukemia in a patient’s blood); 95.5% were MRD-negative when MRD was assessed using protein markers, and 86.4% were MRD-negative when MRD was assessed using DNA markers.
Inotuzumab ozogamicin is given as an intravenous infusion. For the first cycle of treatment, it is recommended that patients be given 0.8 mg/m2 on day 1, 0.5 mg/m2 on day 8, and 0.5 mg/m2 on day 15 of a 21- or 28-day cycle. Dosing beyond the first cycle may vary.
The prescribing information contains a boxed warning for life-threatening liver toxicities and an increased risk of nonrelapse mortality after hematopoietic stem cell transplant.
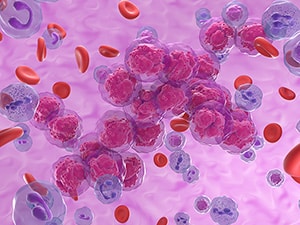
ALL is a type of blood cancer that occurs when the bone marrow makes too many immune cells called lymphocytes. It is most commonly diagnosed among children and young adults under the age of 20. According to federal statistics, it was estimated that 6,540 individuals would be diagnosed with ALL and 1,390 patients would die of the disease in the U.S. in 2023.
The FDA rendered its decision on March 6, 2024.