Targeted Therapy Brentuximab Vedotin Approved for Large B-cell Lymphoma
The FDA has approved the antibody-drug conjugate brentuximab vedotin, plus lenalidomide and rituximab, for certain cases of pretreated large B-cell lymphoma.
The U.S. Food and Drug Administration (FDA) has approved brentuximab vedotin (Adcetris), in combination with lenalidomide (Revlimid) and a rituximab product, for some adult patients with relapsed or treatment-refractory large B-cell lymphoma (LBCL), including diffuse LBCL (DLBCL) not otherwise specified, DLBCL arising from indolent lymphoma, or high-grade B-cell lymphoma. Patients are eligible if they have completed two or more lines of systemic therapy and are ineligible for a stem cell transplant or a type of immunotherapy known as chimeric antigen receptor (CAR) T-cell therapy.
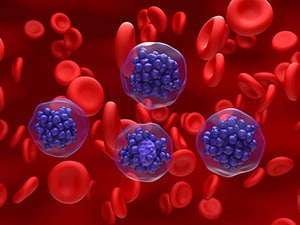
Brentuximab vedotin is a type of targeted therapy known as an antibody-drug conjugate. The antibody component, brentuximab, binds to the protein CD30 on the surface of B cells, including malignant LBCL cells. Upon binding, brentuximab vedotin enters the cell and releases vedotin, a toxic drug that kills the cell.
Lenalidomide is an immunomodulatory drug commonly included in treatment regimens for certain B-cell cancers. Rituximab is an antibody that targets the protein CD30 on B cells and triggers the immune system to destroy them.
Brentuximab vedotin has been previously approved for the treatment of several other types of B-cell lymphoma, as well as certain T-cell lymphomas and cases of mycosis fungoides that express CD30. This is the first approval of brentuximab vedotin for LBCL.
The approval was based on results from the randomized, double-blind, placebo-controlled phase III ECHELON-3 clinical trial. Researchers enrolled 230 patients with LBCL who were ineligible for a stem cell transplant or CAR T-cell therapy and whose LBCL did not respond to or returned after previous treatments. All patients received lenalidomide and rituximab and were randomly assigned (1:1) to also receive brentuximab vedotin or placebo.
Overall, 64.3% of patients in the brentuximab vedotin arm experienced a response, compared with 41.5% of patients in the placebo arm. Patients in the brentuximab vedotin and placebo arms survived for a median of 13.8 months and 8.5 months, respectively. Patients survived without disease progression for a median of 4.2 months in the brentuximab vedotin arm and 2.6 months in the placebo arm.
The prescribing information for brentuximab vedotin includes a boxed warning for progressive multifocal leukoencephalopathy.
The recommended dose of brentuximab vedotin is 1.2 mg/kg, up to a maximum of 120 mg, every three weeks in combination with lenalidomide and rituximab. Treatment may be continued until disease progression or unacceptable toxicity.
LBCL describes a broad subset of non-Hodgkin lymphomas. It includes DLBCL, which is the most common type of non-Hodgkin lymphoma. According to federal statistics, it was estimated that 80,620 individuals would be diagnosed with non-Hodgkin lymphoma and 20,140 patients would die of the disease in the United States in 2024.
The FDA rendered its decision on February 11, 2025. Check this resource for updated information on all therapeutics regulated by the FDA.
