Second Targeted Therapeutic Approved for Use Based on Tumor Biomarker, Not Tumor Origin
Last week, the U.S. Food and Drug Administration (FDA) approved the second of a new wave of molecularly targeted therapeutics that can be used to treat patients with any type of cancer provided their tumor tests positive for a specific biomarker.
The therapeutic in question, entrectinib (Rozlytrek), was approved for treating adults and adolescents age 12 and older whose cancers have an NTRK gene fusion and who have no other effective treatment options.
Entrectinib is the second molecularly targeted therapeutic to be approved for use based on a common biomarker across different types of cancers rather than the location in the body where the cancer originated. It is also the third anticancer therapeutic to be approved for use in this tissue-agnostic way. The first anticancer therapeutic approved for such use was the immunotherapeutic pembrolizumab (Keytruda), in May 2017, for treating certain patients who have solid tumors positive for biomarkers known as microsatellite instability–high or mismatch repair–deficient. The second anticancer therapeutic and the first molecularly targeted therapeutic approved for such use was larotrectinib (Vitrakvi), in November 2018, for treating children and adults who have solid tumors that test positive for the NTRK gene fusion.
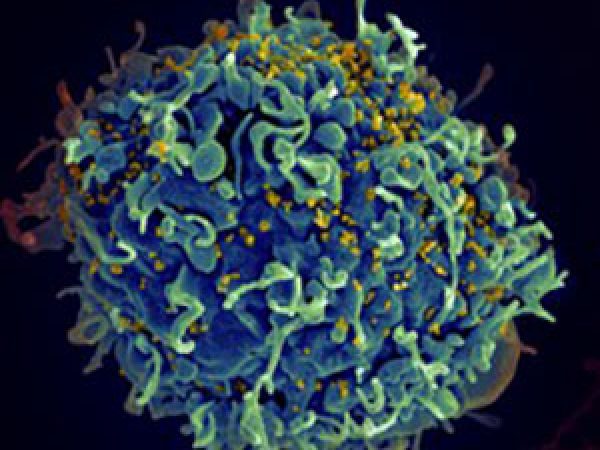
Entrectinib, like larotrectinib, targets three related proteins called TRKA, TRKB, and TRKC, which are encoded by the genes NTRK1, NTRK2, and NTRK3, respectively. Entrectinib also targets ROS1 and ALK proteins.
As discussed in a previous post on this blog, research has shown that genetic alterations known as chromosomal translocations that involve the three NTRK genes and lead to the production of TRK fusion proteins drive the growth of up to 1 percent of all solid tumors. These solid tumors encompass a wide array of cancer types that occur in adults and children, including many rare cancers, such as mammary analogue secretory carcinoma of the salivary gland, infantile fibrosarcoma, and cholangiocarcinoma.
The approval of entrectinib for the treatment of NTRK gene fusion–positive solid tumors was based on integrated data from 54 patients enrolled in one of several phase I and phase II clinical trials. The data, which were presented at the European Society for Medical Oncology (ESMO) 2018 Congress, showed that among 54 patients with NTRK gene fusion–positive solid tumors who were treated with entrectinib, four (7.4 percent) had complete tumor shrinkage and 27 (50 percent) had partial tumor shrinkage. Tumor shrinkage was reported for a range of cancer types, including non–small cell lung cancer (NSCLC), mammary analogue secretory carcinoma of the salivary gland, breast cancer, colorectal cancer, thyroid cancer, pancreatic cancer, and sarcomas.
At the same time as approving entrectinib for the treatment of NTRK gene fusion–positive solid tumors, the FDA also approved the therapeutic for treating adults who have metastatic NSCLC that tests positive for mutations in the ROS1 gene. This approval was based on data from 51 patients who had metastatic ROS1-positive NSCLC who were treated with entrectinib in one of several phase I and phase II clinical trials. Three of the patients (6 percent) had complete tumor shrinkage and 37 (72 percent) had partial tumor shrinkage. Tumor shrinkage persisted for 12 months or longer for 22 of the patients.
Early results from two of the clinical trials on which the entrectinib approvals were based, STARTRK-1 and ALKA-372-001, were presented at the AACR Annual Meeting 2016, as discussed in a previous post on this blog.
At the most recent AACR Annual Meeting, in 2019, researchers reported that a second-generation TRK-targeted therapeutic called LOXO-195 shows early promise against tumors that acquire resistance to first-generation TRK-targeted therapeutics, such as entrectinib. LOXO-195 is just one of many tissue-agnostic anticancer therapeutics in development, as highlighted in a previous post on this blog, a fact that emphasizes how important this approach to cancer treatment will become in the future.
A new molecularly targeted therapeutic for a myeloproliferative neoplasm

Last week, the FDA also approved a new molecularly targeted therapeutic called fedratinib (Inrebic) for treating certain adults with myelofibrosis—specifically, those who have intermediate-2 or high-risk primary or secondary (post-polycythemia vera or post-essential thrombocythemia) myelofibrosis. Primary myelofibrosis, polycythemia vera, and essential thrombocythemia are three of a group of six diseases, including chronic myeloid leukemia, called chronic myeloproliferative neoplasms.
Myelofibrosis is a disease that usually develops slowly. Abnormal blood cells and fibers build up inside the bone marrow, leading to anemia, which in turn causes tiredness, weakness, and shortness of breath. In addition, to make up for the low number of blood cells being made in the bone marrow, the spleen begins to make blood cells, which causes the spleen to enlarge dramatically, a condition known as splenomegaly.
In many patients with myelofibrosis, the disease is driven by mutations in the JAK2 gene. Fedratinib targets JAK2. It was approved for treating myelofibrosis after it was shown in a randomized phase III clinical trial to significantly reduce spleen volume and to reduce myelofibrosis-related symptoms.
A new molecularly targeted therapeutic for a rare cancer
Earlier in August, the FDA approved another new molecularly targeted therapeutic called pexidartinib (Turalio) for treating certain adults with tenosynovial giant cell tumor—specifically, those whose tumor is causing them severe morbidity or functional limitations and is not amenable to surgery.
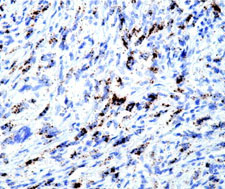
Tenosynovial giant cell tumors are a group of rare tumors that arise in and around the joints and tendons. Although these tumors are benign, they cause damage to the joints, which leads to pain, swelling, and limitation of movement of the joint.
Some cells in tenosynovial giant cell tumors have been shown to harbor chromosomal translocations that lead to overproduction of a protein called CSF1, which attracts large numbers of immune cells. The immune cells that accumulate form the bulk of the tumor and cause damage to surrounding tissue. Pexidartinib targets the protein that CSF1 attaches to on the surface of immune cells, CSF1R, preventing CSF1 from attaching and recruiting the immune cells to the tumor.
Pexidartinib was approved for treating tenosynovial giant cell tumors after it was shown in a randomized phase III clinical trial that 38 percent of patients who received the molecularly targeted therapeutic had complete or partial tumor shrinkage compared with none of the patient who received placebo. The data, which were published recently in Lancet Oncology, also showed that seven patients discontinued pexidartinib because of liver-related adverse effects. As a result, the FDA has mandated that the prescribing information for pexidartinib includes a boxed warning about the risk of serious and potentially fatal liver injury and that pexidartinib only be available through a risk evaluation and mitigation strategy program, which requires that health care providers using pexidartinib be specially certified.
Keeping track of progress
The three new molecularly targeted therapeutics highlighted in this blog brings the total number of new anticancer therapeutics approved by the FDA so far this year to eight. You can read about the other five anticancer therapeutics in the AACR Cancer Progress Report 2019, which will be published September 18, 2019.