Interfacing with the Future: Artificial Intelligence in Oncology
Artificial intelligence (AI) is seemingly everywhere, influencing the hits we get from search engines, the friends and videos we see on social media, and the customer service we receive from businesses.
It’s even impacting how we diagnose and treat cancer.

At the American Association for Cancer Research (AACR) Annual Meeting 2024, researchers discussed AI’s utility for patient care during a plenary session titled “AI at the Interface: Accelerating Evidence Generation, Advancing Disparities Research, and Improving Trial Design.”
While using AI in health care may seem futuristic, “the future is now,” asserted session moderator Vivek Subbiah, MD, chief of early-phase drug development at the Sarah Cannon Research Institute.
“Here, today,” he continued, “we are with AI at the interface.”
What does the interface between AI and cancer care look like? The session’s four speakers discussed current uses of AI and ongoing efforts to improve its future applications—potentially enabling better analyses of medical images, improved risk prediction across the globe, and more precise cancer treatments.
Improving AI’s Ability to Assess Medical Images
AI has been used to analyze medical imaging for the past three decades, said Maryellen Giger, PhD, a professor of radiology at the University of Chicago, as she delivered the first presentation of the session. She explained that AI systems are commonly used to analyze medical images for signs of cancer and cited recent examples of AI systems for imaging-based risk assessment.
But despite their longstanding use in cancer management, Giger noted that AI-based detection tools have several limitations, including inefficiency and lower sensitivity for certain patient populations.
To overcome these issues, she emphasized that existing AI systems should only be used for the specific tasks, populations, and data types for which they were developed, since straying from their intended use can lower accuracy.

For AI systems in development, Giger suggested that developers train AI systems on curated and annotated data from diverse populations. In addition, they should consider the type of information the end user needs (for example, does the user need the AI system to detect cancer, assess risk, or predict therapy response?), the type of data available as input, and the overall design of the clinical study in which the system will be utilized.
“You can have a great AI algorithm, but if you’re using the wrong data to train, [data] that doesn’t match how it will be used eventually, you might blame the algorithm,” said Giger, noting that it was poor data quality with a lack of diversity, rather than poor algorithm design, that hindered AI’s ability to detect infections and predict outcomes during the COVID-19 pandemic.
In response to the obstacles encountered during the pandemic, Giger and colleagues launched the Medical Imaging and Data Resource Center (MIDRC) to facilitate AI development and testing by collecting high-quality and diverse imaging data. While initially formed as an open resource to guide COVID-related AI systems, MIDRC is now collecting imaging data to aid the development of AI systems for cancer detection, risk assessment, and treatment.
“It is important when developing AI for cancer that there is a usable, diverse data set,” said Giger, adding that MIDRC also contains tools to detect and mitigate biases in data sets and to help developers select appropriate performance metrics.
“This is the future of cancer research involving medical images,” she noted.
Addressing Global Health Disparities
While AI is improving the analysis of medical images in some parts of the world, low- and middle-income countries often lack access to imaging technology entirely, according to the session’s second presenter, Anant Madabhushi, PhD, executive director of the Emory Empathetic AI for Health Institute at the Winship Cancer Institute of Emory University.
Some countries also have a limited number of pathology experts to interpret tissue histology, which means that both imaging- and histology-based risk prediction models are out of reach for many patients in these regions.
But AI has the power to bring risk prediction—and the enhanced treatment decision-making that comes with it—to low-resource settings, Madabhushi noted.
He explained that a form of AI known as digital pathology could allow clinicians to simply upload images of tissue histology slides into a computer program and receive an AI-based assessment of the slide.
In his presentation, Madabhushi showed that a digital pathology algorithm assessing collagen disorder in breast tissue accurately predicted survival outcomes in patients with breast cancer while having a lower cost, shorter turnaround time, and greater accessibility than Oncotype DX, a genomic-based risk prediction model routinely used in the United States.
Given recent reports suggesting that Oncotype DX is less accurate for Black patients, Madabhushi echoed Giger’s sentiments about the importance of training new AI models on diverse patients, particularly if they are intended to be used across the globe.
“As we think about the opportunity for artificial intelligence in precision medicine … we also have to be thinking about it from a global context,” he said. “We have to be intentional and make sure that these AI technologies work across diverse populations.”
Matching Targeted Therapies to Patients
In precision medicine, understanding the molecular underpinnings of each patient’s cancer is a key step to selecting appropriate targeted therapies. Current methods rely heavily on identifying a cancer’s genetic alterations, but Thomas Clozel, MD, co-founder and chief executive officer of Owkin, argued that this approach is insufficient.
With current methods, he explained, fewer than 10% of patients benefit from targeted therapy even when receiving therapy matched to their tumor’s genetic mutation. He argued that AI algorithms could improve patient stratification and enable more precise therapies. But the development of such algorithms will require a much deeper understanding of tumor biology and substantially more data.
“To discover something new, we need a lot of data—10 times more than what you’ve been reading in any paper,” he said.
An obstacle facing developers is that patient data, rightfully so, are kept confidential, Clozel noted. This makes it difficult to generate a sufficiently large and diverse data set upon which to build an AI model.
To overcome this barrier, Clozel and colleagues are employing federated learning, wherein patient data remain secure within their original location, but the AI algorithms based on data at each site are shared between institutions.
“When you do this, you break research silos,” while maintaining patient and physician trust, said Clozel. “Federated learning is key to being able to access data at scale.”
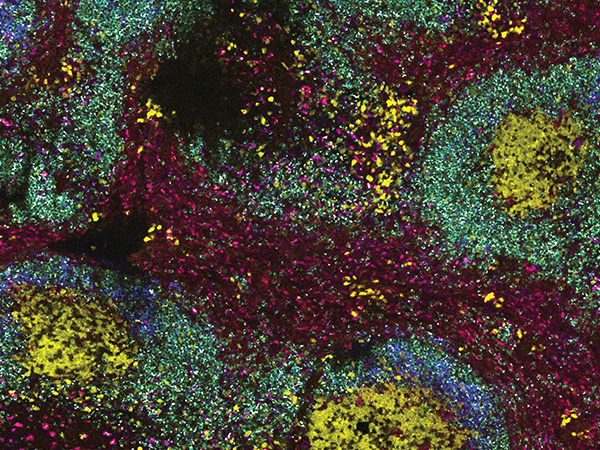
Clozel also stressed the importance of understanding spatial biology—how cancer cells interact with other cells within the tumor microenvironment—to identify new therapeutic targets. Unfortunately, he noted, existing spatial biology data sets are too small to enable significant breakthroughs.
Therefore, Clozel and colleagues developed MOSAIC, a large atlas of spatial biology data from approximately 7,000 patients representing seven different cancer types. MOSAIC incorporates data from spatial transcriptomics, single-cell RNA sequencing, bulk RNA sequencing, whole exome sequencing, tissue histology, and the clinic. It is intended to guide the development of AI tools that analyze spatial biology data to discover new precision medicine approaches.
Finally, Clozel shared examples of predictive AI tools that he and colleagues have developed, including MesoNet to predict the survival of patients with mesothelioma, HCCNet to predict prognosis of patients with liver cancer, and RlapsRiskBC to identify breast cancer patients with a high risk of relapse.
A Pan-tumor Model to Identify Homologous Repair Deficiency
In the final presentation, Mia Levy, MD, PhD, chief medical officer of Foundation Medicine, discussed the development and validation of HRDsig, an AI algorithm to identify tumors with homologous repair deficiency (HRD).

Tumors with HRD have impaired DNA repair and are susceptible to targeted therapies that work through synthetic lethality. Traditionally, HRD has been identified by looking for mutations in certain genes, such as BRCA, but these methods may miss HRD caused by mutations in other genes, Levy noted. HRDsig, in contrast, works by looking for tumor agnostic “genomic scars” caused by HRD, including loss of heterozygosity, telomere allele imbalances, and other copy number changes.
The algorithm was built using over 100 copy number changes and was trained on data from over 500,000 patients. In validation studies of patients with ovarian, prostate, breast, or pancreatic cancer, HRDsig detected over 75% of tumors with biallelic loss of BRCA and identified tumors with other HRD-causing gene alterations.
Compared to BRCA mutation alone, HRDsig identified up to twice as many patients who could have benefitted from PARP inhibition in retrospective studies, including patients with ovarian, colorectal, breast, and other cancers. These results suggest that HRDsig could be used across tumor types to better stratify patients for PARP inhibition or other DNA repair-targeted therapies, and a prospective study to evaluate its predictive capability has been initiated.
“I encourage all of us to keep a high standard … for these AI-generated approaches,” Levy concluded. She argued that, although vigorous validation can be expensive, it is needed to ensure the accuracy of new AI tools.
“Without the rigor, we risk just getting excited about the trendy term ‘AI,’” she said. “I think we’ve seen from our speakers today and from this example that we’re still holding [AI] to a high standard.”
Learn more about AI in clinical practice in a recent review article in Cancer Discovery, a journal of the AACR. To learn about AI in oncology drug development, check out our interview with drug discovery expert Paul Workman, PhD.